EXPOSURE PREVENTION
It is important for all healthcare workers to understand the role they play in protecting themselves, coworkers, patients, and families from exposure to bloodborne pathogens. The employer’s exposure control plan provides the following detailed information about how each healthcare worker can take appropriate steps to reduce or eliminate the risk of exposure to bloodborne pathogens as well as other infectious agents.
Universal and Standard Precautions
Universal Precautions is the term used to describe a prevention strategy in which all blood and OPIM are treated as if they are actually infectious, regardless of the perceived status of the source individual. In other words, whether or not one thinks the blood or body fluid is infected with bloodborne pathogens, treat it as if it is. This approach is used in all situations where exposure to blood or OPIM is possible. In addition, certain engineering and work practice controls are always utilized in situations where exposure may occur.
OSHA’s Bloodborne Pathogens Standard allows for healthcare facilities to use acceptable alternatives to Universal Precautions. The CDC revised the infection control practice from Universal Precautions to Standard Precautions in 1996. Standard Precautions combine the major features of Universal Precautions with body substance isolation (BSI). Standard Precautions incorporate not only the fluids and materials covered by the Bloodborne Pathogens Standard but expand coverage to include any and all body fluids and substances (OSHA, 2019).
These precautions are intended to address all modes of transmission by any type of organism. Routes of transmission may be direct or indirect.
- Direct transmission is the immediate transfer of microorganisms from one infected person to another without a contaminated intermediate object or person, including:
- Direct contact, such as skin to skin
- Direct projection of a spray of droplets, such as coughing, sneezing, speaking, or spitting onto a close contact
- Inoculation into skin or mucosa, such as through contaminated needles
- Indirect transmission includes a variety of mechanisms and requires that the infectious agent is capable of surviving outside the host in the external environment:
- Vehicle borne, such as through water, food, ice, blood, plasma, and other biological products
- Vector borne, such as by an arthropod or any living carrier
- Airborne by evaporation of droplets that are coughed or sneezed into the air or generated purposefully by atomizing devices and disseminated by air currents and that can remain suspended in air for hours or settle and become part of dust
- Fomite (inanimate articles or substances) borne, such as clothing, utensils, and furniture that are contaminated by infectious substances and capable of harboring and transferring the agent
Standard Precautions for Bloodborne Pathogens
The Standard Precautions that are to be followed by all healthcare workers when concerned with bloodborne pathogens or other potentially infectious materials include:
- Performing hand hygiene
- Using personal protective equipment (PPE) whenever there is an expectation of possible exposure to infectious material
- Following respiratory hygiene or cough etiquette principles
- Ensuring appropriate patient placement
- Properly handling and properly cleaning and disinfecting patient-care equipment and instruments or devices; appropriate cleaning and disinfecting of the environment
- Handling textiles and laundry carefully
- Safe injection practices
- Infection control practices for special lumbar procedures
- Ensuring healthcare safety by proper handling of regulated waste, including proper handling of needles and other sharps
(CDC, 2023b)
HAND HYGIENE
Hand hygiene involves cleaning hands with soap and water, antiseptic hand wash, antiseptic hand rub, or surgical hand antisepsis. Hands should be washed with soap and water whenever they are visibly dirty, before eating, and after using the restroom. Alcohol-based hand sanitizers are the preferred method for cleaning hands in most clinical situations.
Using an alcohol-based hand sanitizer or handwashing with soap and water is to be performed:
- Immediately before touching a patient
- After contact with blood, body fluids or excretions, mucous membranes, nonintact skin, or wound dressings
- After contact with a patient’s intact skin
- If hands will be moving from a contaminated body site to a clean body site
- After contact with inanimate objects in the immediate vicinity of the patient
- When hands are visibly soiled
- Before performing an aseptic task or handling invasive medical devices
- After caring for a person with known or suspected infectious diarrhea
- Immediately after glove removal
(CDC, 2023b)
Recommendations regarding fingernails state:
- Do not wear artificial fingernails or extenders if duties include direct contact with patients at high risk for infection and associated adverse outcomes (e.g., those in ICUs or ORs).
- Keep natural nail tips less than 1/4-inch long.
(CDC, 2023b)
HAND HYGIENE WITH SOAP AND WATER OR HAND SANITIZER
The CDC guidelines for hand hygiene in healthcare settings recommend:
When using soap and water:
- Wet hands with clean running water (warm or cold), turn off the tap, and apply soap.
- Lather hands by rubbing them together. Lather the back of the hands, between fingers, and under nails.
- Scrub hands for at least 20 seconds.
- Turn on the tap with elbow or disposable towel.
- Rinse hands well under clean running water.
- Dry hands using a disposable towel or air dryer.
- Use a clean disposable towel to turn off the faucet.
When using an alcohol-based hand sanitizer:
- Apply the amount of product recommended by the manufacturer to the palm of one hand.
- Cover all surfaces of hands.
- Rub the product over all the surfaces of the hands and fingers until hands are dry; this should take about 20 seconds.
(CDC, 2022c)
PERSONAL PROTECTIVE EQUIPMENT (PPE)
To protect oneself, healthcare providers must have a protective barrier between them and any potentially infectious material. Personal protective equipment is defined by OSHA as specialized clothing or equipment worn by a healthcare worker for protection against infectious materials.
Employers are required to provide and maintain clean, appropriate PPE at no cost to employees. Latex-free PPE must be made available on request. PPE must be readily accessible to employees and available in appropriate sizes. It is important to know which type of PPE is available at work and where it is stored.
Types of PPE used in healthcare settings to protect healthcare workers from exposure to bloodborne pathogens include:
- Gloves
- Gowns, aprons, coveralls, laboratory coats
- Masks, face shields, goggles
- Ventilation devices (mouthpieces, pocket masks, resuscitation devices)
- Head coverings
- Boots or shoe covers
- Respirators
Factors that influence the selection of appropriate PPE include:
- Type of exposure anticipated
- Splash or spray versus touch
- Category of isolation precautions (Contact, Droplet, Airborne)
- Durability and appropriateness for the task
- Fit of the equipment
Gloves
Gloves are the most common type of PPE and are not a substitute for hand hygiene. They are used for patient care as well as when contacting environmental services. Gloves can be sterile or nonsterile and single-use or reusable. Because of allergy concerns, latex products have been eliminated in many facilities, and materials used for gloves are mostly synthetics such as vinyl or nitrile.
- Wear gloves when reasonably anticipated that contact with blood or OPIM, mucous membranes, nonintact skin, or potentially contaminated intact skin could occur.
- Wear gloves with fit and durability appropriate to the task.
- Wear disposable medical examination gloves for direct patient care.
- Wear disposable medical examination gloves or reusable utility gloves for cleaning environment or medical equipment.
- Remove gloves after contact with a patient or the surrounding environment (including medical equipment) using proper technique to prevent hand contamination.
- Never wear the same pair of gloves for the care of more than one patient.
- Never wash patient-care gloves for reuse.
- Change gloves during patient care if hands will move from a contaminated body site to a clean body site.
(CDC, 2023b)
Gowns
Gowns appropriate to the task are worn to protect skin and prevent soiling or contamination of clothing during procedures and patient-care activities when contact with blood, body fluids, secretions, or excretions is anticipated.
- Wear a gown for direct patient contact if the patient has uncontained secretions or excretions.
- Remove a gown and perform hand hygiene before leaving the patient’s environment.
- Do not reuse gowns, even for repeated contacts with the same patient.
Routine donning of gowns upon entrance into a high-risk unit (e.g., ICU, NICU, HSCT unit) is not indicated (CDC, 2023b).
Mouth, Nose, and Eye Protection
Face and eye protection, including masks, goggles, face shields, and combinations of each, are selected according to the needs anticipated by the task to be performed to protect the mucous membranes of the eyes, nose, and mouth during procedures and patient-care activities that are likely to generate splashes or sprays of blood, body fluids, secretions, and excretions.
During aerosol-generating procedures in patients who are not suspected of being infected with an agent for which respiratory protection is otherwise recommended (e.g., tuberculosis), wear one of the following in addition to gloves and gown:
- A face shield that fully covers the front and sides of the face
- A mask with attached shield
- Mask and goggles
(CDC, 2023b)
Head Coverings
Head coverings such as surgical caps are worn when gross contamination is expected, such as during orthopedic surgery or autopsies (OSHA, 2019).
Boots or Shoe Covers
Theater boots are waterproof boots worn by surgical personnel as a protective measure from contamination with blood and other body fluids. Shoe covers protect the wearer from accidental spills and body fluids (OSHA, 2019).
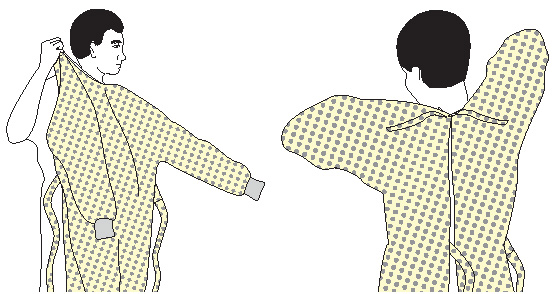
DONNING PPE
There are various ways to don PPE. The CDC recommends that PPE be put on in the following sequence:
- Gown
- Mask
- Face shield or goggles
- Gloves
How to put on a gown:
- Perform hand hygiene using hand sanitizer.
- Select appropriate type and size.
- Put on with opening in the back.
- Secure at neck and waist.
- If gown is too small, use two gowns, with the first tied in front and the second tied in back.
How to put on a mask:
- Place over nose, mouth, and chin.
- Fit flexible nose piece over bridge of nose using both hands.
- Ensure facemask extends under the chin.
- Secure on crown of the head and base of the neck. If mask has loops, hook them around the ears.
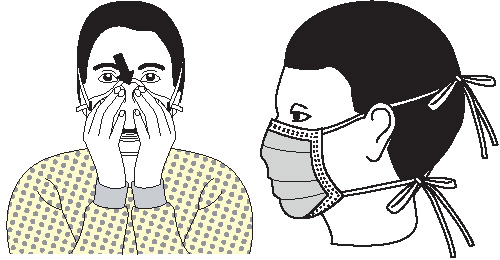
How to put on goggles and face shield:
- Place over face and eyes.
- Adjust to fit.

How to put on gloves:
- Select correct type and size.
- Insert hands into gloves.
- Extend gloves over isolation gown cuffs.
(CDC, 2020b)
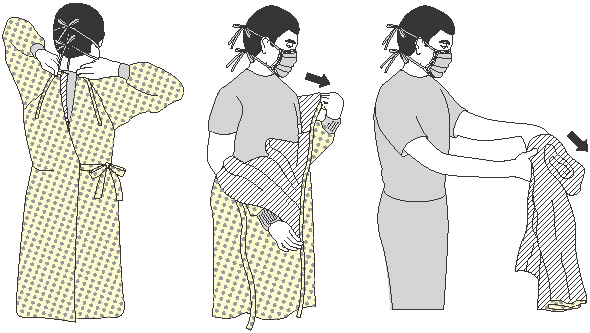
DOFFING PPE
More than one doffing method may be acceptable. Training and practice using the healthcare facility’s procedure is critical. One example of removing PPE is described below.
Remove contaminated PPE in the following sequence:
- Gloves
- Gown
- Face shield or goggles
- Mask or respirator
PPE is to be removed at the doorway before leaving the patient room or in the anteroom. Respirators are removed outside the room after the door has been closed.
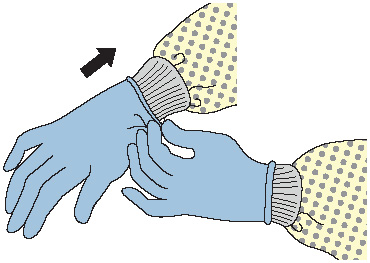
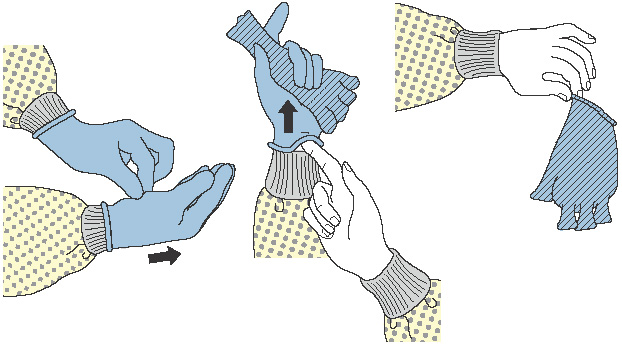
How to remove gloves:
- Grasp outside edge near wrist.
- Peel away from hand, turning glove inside out.
- Hold in opposite gloved hand.
- Slide ungloved finger under wrist of remaining glove.
- Peel off from inside, creating a bag for both gloves.
- Discard.
- Perform hand hygiene if contamination occurs during glove removal.
How to remove gown:
- Consider gown front and sleeves to be contaminated.
- Unfasten ties. (Some gown ties can be broken rather than untied.)
- Pull gown away from neck and shoulders, touching inside of gown only.
- Turn contaminated outside toward the inside and over the hands.
- Fold or roll into a bundle and discard.
- Perform hand hygiene if contamination occurs.
How to remove goggles or face shield:
- Consider outside of goggles or face shield to be contaminated.
- Remove from the back by lifting head band or ear pieces.
- Lift away from face.
- Place in the designated receptacle for reprocessing or disposal.
- Perform hand hygiene if contamination occurs.

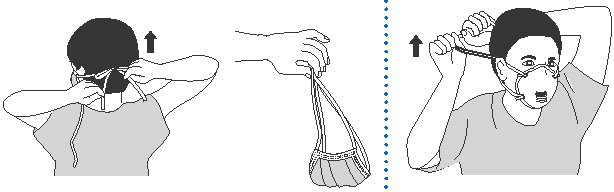
How to remove mask:
- Consider the front of the mask to be contaminated; do not touch.
- Carefully untie bottom ties, then upper ties, or unhook from ears and pull away from face.
- Discard.
- Perform hand hygiene before exiting the patient area.
(CDC, 2020b)
CLEANING AND DISINFECTING
All equipment and environmental and working surfaces must be cleaned and decontaminated after contact with blood or other potentially infectious material. Protective gloves and other PPE should be worn as necessary, and an appropriate disinfectant should be used.
When cleaning up a blood spill or OPIM, use protective gloves or other PPE as necessary and:
- Confine the spill and immediately wipe it up with absorbent (paper) towels, cloths, or absorbent granules that are spread over the spill to solidify the blood or body fluid. Dispose of all as infectious waste.
- Clean up all blood thoroughly using neutral detergent and warm water solution before applying the disinfectant.
- Disinfect by using a facility-approved intermediate-level disinfecting solution; typically, chlorine-based disinfectants are adequate for disinfecting spills.
- When using a diluted bleach solution, contact time is the length of time it takes for the solution to dry. (Do not use a diluted bleach solution to clean up a urine spill due to risk of chlorine gas.)
- Allow disinfectant to remain wet on the surface for the recommended contact time, then rinse the area with clean water to remove the disinfectant residue (if required).
- Immediately send all reusable supplies and equipment (e.g., cleaning cloths, mops) for reprocessing (i.e., cleaning and disinfection) after the spill is cleaned up.
Liquid chlorine bleach comes in different concentrations. To make a 0.5% chlorine solution from 3.5% bleach, use 6 parts of water per 1 part bleach (CDC, 2023c).
HANDLING CONTAMINATED LAUNDRY
Contaminated laundry (i.e., soiled with blood or OPIM or that may contain sharps) should be handled as little as possible and should not be sorted or rinsed in the location of use. Contaminated laundry is bagged at the location of use into labeled or color-coded bags or containers. Contaminated laundry that is wet is placed and transported in containers or bags that prevent soak-through or leakage (OSHA, 2019).
HANDLING REGULATED WASTE
Regulated waste refers to:
- Any liquid or semiliquid blood or other OPIM
- Contaminated items that would release blood or OPIM in a liquid or semi-liquid state if compressed
- Items that are caked with dried blood or OPIM and are capable of releasing these materials during handling
- Contaminated sharps
Regulated waste shall be placed in containers which are closable; constructed to contain all contents and prevent leakage of fluids during handling, storage, transport, or shipping; and labeled or color-coded in accordance with the OSHA Standard.
If outside contamination of the regulated waste container occurs, place it in a second container, close, and color-code or label with biohazard symbols (OSHA, 2019).
Sharps Handling
Contaminated sharps are needles, blades (such as scalpels), scissors, and other medical instruments and objects that can puncture the skin. Contaminated sharps must be properly disposed of immediately or as soon as possible into containers that are closable, puncture-resistant, leak-proof on the sides and bottom, and color-coded or labeled with a biohazard symbol.
HOW TO HANDLE SHARPS
- Discard needle or syringe units without attempting to recap the needle whenever possible.
- If a needle must be recapped, never use both hands; use the single-hand “scoop” method.
- Never break or shear needles.
- To move or pick up needles or other sharp devices, use a mechanical device or tool, such as forceps, pliers, or broom and dustpan.
- Dispose of needles in labeled sharps containers only; sharps containers must be accessible and maintained upright. When transporting sharps containers, close the containers immediately before removal or replacement to prevent spillage or protrusion of contents during handling or transport.
(OSHA, 2019)