HIV/AIDS ETIOLOGY AND PATHOGENESIS
HIV, the human immunodeficiency virus, spreads via certain body fluids; specifically attacks the CD4, or T cells, of the immune system; and uses those cells to make copies of itself. CD4 cells, also called helper T cells, are a class of white blood cells that help other lymphocytes (memory B cells) that are responsible for producing an antibody to fight infection based on stored data following past exposure to the antibody. As time passes, the virus can destroy enough of these specialized cells that the immune system no longer is able to fight off infections and disease.
HIV is unique among many other viruses because the body is unable to destroy it completely, even with treatment. As a result, once a person is infected with the virus, the person will have it for the remainder of their life (CDC, 2022b).
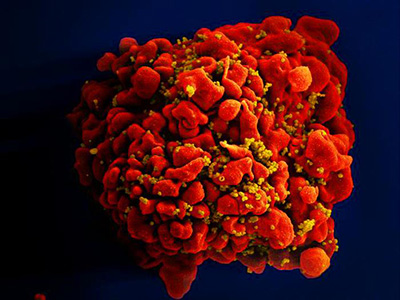
A single T cell (red) infected by numerous, spheroid shaped HIV particles (yellow). (Source: National Institute of Allergy and Infectious Diseases, 2012.)
After the initial infection and without treatment, the virus continues to multiply, and over a period of time (which can be 10 years or longer), common opportunistic infections (OIs) begin to take advantage of the body’s very weak immunity. When an opportunistic infection occurs, the person has developed acquired immunodeficiency syndrome (AIDS). Today, OIs are less common in people with HIV because of effective treatment (CDC, 2021a).
Origin and Strains of HIV
Human immunodeficiency virus came from a specific type of chimpanzee in Central Africa and may have jumped from these animals to humans as far back as the late 1800s. The virus has existed in the United States since at least the mid to late 1970s. HIV infection is caused by the HIV-1 or HIV-2 retroviruses in the Retroviridae family, Lentivirus genus.
Of the two main types of human immunodeficiency virus, HIV-1 is the most common; HIV-2 occurs in fewer people. HIV-2 is harder to transmit from one person to another, and it takes longer for the infection to advance to AIDS. Both strains have different groups within them.
HIV-1 includes four groups, with group M responsible for nearly 90% of all HIV-1 cases. This group has nine different strains, and some of these have sub-strains. New strains are being discovered all the time. The B strain is the most common in the United States. The most common HIV strain worldwide is C. The groups N, O, and P are rare outside of west Central Africa.
HIV reproduces carelessly, accumulating many mutations when copying its genetic material, and reproduces at an extremely fast rate. One single virus can produce billions of copies in just a single day (CDC, 2022b; UCB, 2023; Ellis, 2022).
Disease Pathogenesis
The distinguishing characteristic of human immunodeficiency viral infection is the gradual loss of CD4 cells and an imbalance in CD4 cell homeostasis, with progressive impairment of immunity that eventually culminates in death.
HIV is unable to grow or reproduce on its own and depends on a host cell for the raw materials and energy necessary for all the biochemical activities that allow the virus to reproduce. In order to accomplish this, it must locate and bind to a specific type of cell, the CD4 T cell.
The HIV life cycle involves seven stages:
- Binding: HIV attacks a CD4 cell and attaches itself to its protein molecules.
- Fusion: After attaching to the CD4 cell, the HIV viral envelop fuses with the cell membrane, allowing the virus to enter the cell and release HIV RNA and HIV enzymes.
- Reverse transcription: Once inside the cell, HIV releases and uses reverse transcriptase to convert its genetic material (HIV RNA) into HIV DNA, allowing HIV to enter the cell nucleus and combine with the cell’s DNA.
- Integration: Inside the cell’s nucleus, HIV releases integrase, an HIV enzyme, to insert its viral DNA into the DNA of the host cell.
- Replication: When the virus is integrated into the host cell DNA, it begins to use the machinery of the cell to create long chains of HIV proteins, building blocks for more HIV. This results in the death of the CD4 cell.
- Assembly: During assembly, new HIV RNA and HIV proteins made by the host cell move to the surface and assemble into immature noninfectious HIV.
- Budding: Immature HIV pushes itself out of the host cell and releases an enzyme that breaks up the protein chains in the immature virus, creating the mature infectious virus.
When the mature infectious virus enters the bloodstream, the new virus repeats the process, further depleting the CD4 count and effectively reducing immunity (NIH, 2021).