COMPONENTS OF BALANCE
It is commonly accepted that falling is often, if not nearly always, the result of “losing one’s balance.” But what exactly does balance mean and how does its presence or absence contribute to falls?
Defining “Balance”
Balance refers to the ability of an individual to maintain their line of gravity within an established base of support. Alternatively, balance may be described as being able to maintain one’s equilibrium, or a state in which all acting forces cancel one another and create a stably balanced system. Postural control, postural stability, and equilibrium are alternative terms for balance (Physiopedia, 2023a).
Static balance is the ability of the body to be held in a fixed (unmoving) position, maintaining postural orientation and stability with the body at rest and the center of mass held over the base of support. Dynamic balance, in contrast, is the ability to maintain stability and orientation of one’s posture while the body is in motion (Bannister, 1969, quoted in Physiopedia, 2023a).
Systems of Balance
When properly functioning, the human balance systems allow individuals to:
- Clearly see surroundings while in motion
- Determine orientation with respect to gravity
- Interpret the speed and direction of movement
- Make continuous and automatic adjustments to posture
These abilities contribute to maintaining stability while engaging in various activities under varying environmental conditions (VeDA, 2023a).
Balance, or the lack thereof, is thus not a function of merely one discrete component but is the result of input from several distinct sensorimotor control systems within the human body that work synergistically. The ability of an individual to maintain balance is controlled by integrated sensory input from vision, proprioception, and the vestibular system, with subsequent motor output to the muscles of the eyes and body. If one or all of these components is adversely affected (which may be caused by factors such as disease, injury, aging, or drugs), an individual’s overall balance may become compromised (VeDA, 2023a; Physiopedia, 2023a).
VISUAL SYSTEM
The retinae of the eyes contain rods (for vision in low-light situations) and cones (for color and fined-tuned vision). When struck with light, these structures convey impulses to the brain with visual cues regarding how the body is orientated relative to surrounding objects. The visual system provides approximately 10% of total balance input on stable surfaces and 30% on unstable surfaces.
Many different visual dysfunctions contribute to problems with balance. A few examples include:
- Aniseikonia: A condition in which there is a significant difference in how an individual’s right versus left eye perceives an image’s size, which may cause disorientation, eyestrain, headache, and/or issues with dizziness and balance.
- Vertical imbalance: A condition in which one eye aims higher than the other instead of both eyes working in synchrony. An affected person will frequently tilt their head to help align the eyes in order to try to compensate for this vertical maladjustment, which may then adversely affect the vestibular fluid of the inner ear.
- Binocular vision dysfunction: A condition in which the eyes struggle to work together when aiming or focusing at a point in space or when quickly changing gaze between closer and farther objects. It may be caused by brain injury to specific neural centers and can lead to eye teaming/focusing issues, resulting in double or blurry vision.
(NORA, 2023)
SOMATOSENSORY/PROPRIOCEPTIVE SYSTEM
Proprioceptive information from the skin, muscles, and joints involves sensory receptors that are sensitive to stretch or pressure in the surrounding tissues. Proprioceptive cues help a person’s body determine its position in space. Of particular importance to balance, cues from the neck indicate the direction the head is turned, and cues from the ankles indicate body movement and/or sway relative to the standing surface and its quality (soft, uneven, solid, etc.). The somatosensory/proprioceptive systems provide approximately 70% of total balance input on stable surfaces and 10% on unstable surfaces (VeDA, 2023a; Physiopedia, 2023a).
Problems related to the somatosensory/proprioceptive systems may adversely affect balance. For example:
- Impaired cervical range of motion is associated with diminished protective responses and/or balance. Patients with cervical pain/dysfunction often experience symptoms of dizziness/light-headedness and/or unsteadiness, which lead to increased fall risk (Sung, 2020).
- Loss of ankle range of motion and proprioception after ankle injury has been shown to adversely impact postural and balance control, and athletes with impaired ankle proprioception post injury tend to perform more poorly in both static and dynamic postural and balance control tasks (Alghadir et al., 2020).
- Sensory impairments such as diabetic peripheral neuropathy have been shown both to significantly diminish an individual’s functional balance and to increase their risk of falls (Reeves et al., 2021).
VESTIBULAR SYSTEM
The vestibular apparatus is located within each inner ear. It includes the utricle, saccule, and three semicircular canals and provides sensory information regarding equilibrium, motion, and spatial orientation. The utricle and saccule detect linear movement and vertically oriented input (i.e., gravity), while the semicircular canals detect rotational movement.
The semicircular canals are located at right angles to one another and are filled with endolymphatic fluid. When the head is turned in certain directions, the endolymphatic fluid in the corresponding semicircular canal moves more slowly due to inertia, placing pressure against the canal’s sensory receptor, which subsequently sends impulses to the brain specifically about the movement occurring in that particular canal.
When the vestibular system is functioning correctly, these impulses are symmetrical to both sides of the head. The vestibular system provides approximately 20% of total balance input on stable surfaces and 60% on unstable surfaces (VEDA, 2023b).
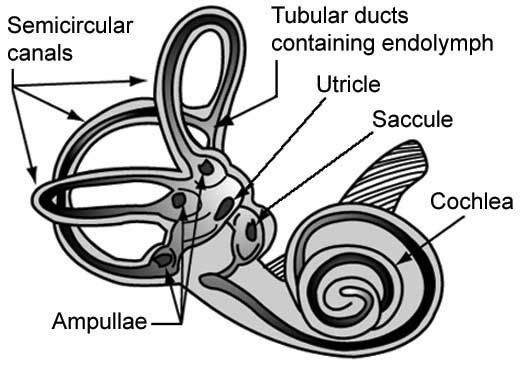
Vestibular system. (Source: NASA.)
There are a number of conditions that can cause vestibular system dysfunction, which may in turn lead to dizziness or affect balance. Some examples include:
- Benign paroxysmal positional vertigo (BPPV): The most common cause of vertigo, BPPV is a mechanical problem that occurs when calcium carbonate crystals (called canaliths or otoliths) become displaced in the inner ear, stimulate nerve hairs, and send false movement signals to the brain, which can cause dizziness and visual disturbance. This may occur as a result of infection, trauma, or normal aging.
- Acoustic neuroma: Nonmalignant tumor that develops on the sheath of the inner ear’s vestibulocochlear nerve. Also known as vestibular schwannoma.
- Autoimmune inner ear diseases: Includes Cogan’s syndrome, relapsing polychondritis, polyarteritis nodosa, Wegener’s granulomatosis, systemic lupus erythematosus, ulcerative colitis, Sjogren’s syndrome, and rheumatoid arthritis.
- Cholesteatoma: A skin growth that occurs in the middle ear behind the eardrum; can increase in size and destroy middle ear structures over time.
- Labyrinthitis and vestibular neuritis: Disorders resulting from an infection of the inner ear or the nerves connecting the inner ear and brain, disrupting transmission of sensory information.
- Mal de débarquement syndrome (MDDS): Most commonly occurs after sea or other forms of travel; the sensation of movement continues after movement has stopped. Cause not definitely known, may last for weeks, months, or even years.
- Migraine associated vertigo (MAV): Approximately 40% of migraine patients have some accompanying vestibular syndrome involving disruption in their balance and/or dizziness; thought to be a combination of altered vascular and neural processes.
- Otosclerosis: Abnormal bone growth in the middle ear, which can cause hearing loss, dizziness, balance problems, or tinnitus.
- Ototoxicity: Poisoning that results from exposure to drugs or chemicals that damage the inner ear or the vestibulocochlear nerve; may be temporary or permanent.
- Perilymph fistula: A tear or defect in either or both the oval window and the round window that separate the middle and inner ear, allowing perilymph to leak into the middle ear. Most frequently caused by head trauma (such as a direct blow or a whiplash injury). Other causes include ear trauma, perforated eardrum, “ear block” during airplane descent, or scuba diving.
- Persistent postural perceptual dizziness (PPPD): Postural dizziness without vertigo and fluctuating unsteadiness provoked by environmental or social stimuli (e.g. crowds), not attributable to another neuro-otologic disorder.
(VEDA, 2023c)
VERTIGO VS. DIZZINESS
While the terms are often used interchangeably, these are two distinct symptoms. Dizziness can refer to a general feeling of feeling off-balance, or like you are about to fall. Vertigo, in contrast, is a sense of feeling as though you or your surroundings are actually moving (Healthline, 2023).