PREGNANCY-RELATED BLEEDING COMPLICATIONS
Vaginal bleeding during pregnancy must always be investigated, particularly if it is enough blood to drop into the toilet or to warrant use of a menstrual pad. Bleeding can indicate pregnancy loss, placenta previa, placental abruption, ectopic pregnancy, or gestational trophoblastic disease. Events that may result in a small amount of bleeding (perhaps seen on toilet paper after voiding) due to cervical irritation include recent vaginal intercourse or recent cervical exam.
Pregnancy Loss
Pregnancy loss (also referred to as spontaneous abortion or miscarriage) is defined as a nonviable intrauterine pregnancy less than 20 weeks’ gestation (Prager et al., 2022b). This loss occurs without intervention from the patient or another person.
Pregnancy loss affects 10%–31% of pregnancies (Prager et al., 2022a). Risk for pregnancy loss increases with increasing maternal age and prior pregnancy loss. Pregnancy loss can be caused by a number of other factors, including chromosomal abnormalities, maternal infection, maternal endocrine disorders (e.g., hypothyroidism, uncontrolled diabetes), reproductive system abnormalities (e.g., cervical insufficiency), substance use, environmental factors (exposure to toxins and pollutants), and maternal injury.
NURSING CARE
The primary nursing intervention for all types of pregnancy loss is to ensure patient safety by identifying and controlling any bleeding and hemorrhagic shock. Symptoms of hemorrhagic shock include an increased heart rate, decreased blood pressure, cool and clammy skin, lightheadedness, and confusion. The nurse should anticipate the need for oxygen therapy and fluid and blood replacement. Patients should be blood-typed and cross-matched in case blood transfusion is necessary.
Pregnancy loss may be managed expectantly, with medication, or with surgery. Medication administration may include misoprostol (Cytotec) with or without the use of a prior dose of methotrexate. Misoprostol may be used to help in expelling the pregnancy tissue or to control bleeding. A patient-centered approach is recommended. By encouraging patients to participate in decision making about their care, they are likely to feel more satisfied.
The nurse monitors the patient’s vital signs, oxygen saturation, intake and output, and laboratory results according to institutional policies. If a patient experiences a threatened abortion but the fetus does not die, the nurse may be responsible for monitoring fetal heart sounds and the overall well-being of the fetus depending on gestational age. The nurse should administer prescribed anti-D-immune globulin (human) (RhoGAM) to Rh-negative patients within 72 hours to prevent alloimmunization (an immune response to the fetus’s blood cells).
RhoGAM
RhoGAM should be given to Rh-negative patients at approximately 28 weeks’ gestation, within 72 hours of the birth of an Rh-positive baby, with the possibility of maternal fetal hemorrhage (such as trauma to the abdomen during pregnancy, after an ectopic pregnancy, bleeding during pregnancy, after a pregnancy loss or induced abortion, after attempt at cephalic version, and after invasive procedures [e.g., amniocentesis]).
COMPLICATIONS
Two serious complications of missed abortions are infection and disseminated intravascular coagulation (DIC). Infection can occur as a result of carrying an expired fetus and is a serious health threat to these patients. DIC produces clotting, bleeding, and ischemia that occur simultaneously. Symptoms include sudden shortness of breath, chest pain, and/or cyanosis. Bleeding from the nose, gums, and IV sites, as well as petechiae, also occur in the presence of DIC. Treatment is aimed at delivering the fetus and placenta, which will stop the overactivation of the clotting process. Patients are treated with oxygen therapy and are usually given blood products.
| Normal in Pregnancy | DIC | |
|---|---|---|
| * Made when clots are broken down (Cunningham, 2022) |
||
| Fibrinogen (factor I) | 244–696 mg/dL | ⇓ |
| Platelets | 146–429 x109/L | ⇓ |
| D-dimer* | 200–1600 ng/mL | ⇑ |
PATIENT TEACHING
Nurses are responsible for ensuring that patients are adequately prepared to care for themselves upon discharge from the hospital following treatment or monitoring for a pregnancy loss. It is important that patients understand the warning signs of further complications and the importance of reporting such signs to their healthcare practitioner.
Warning signs include fever, foul-smelling vaginal discharge, significant bright-red vaginal bleeding, and pelvic pain. In addition, patients are encouraged to maintain pelvic rest (nothing per vagina) for two weeks. Experiencing a pregnancy loss is challenging for women both physically and emotionally, and they need to rest for a few days after discharge. They may be prescribed iron supplements for blood loss and/or antibiotics to treat or prevent infection. Foods such as liver, green leafy vegetables, dried foods, and eggs provide needed iron. Additional fluid intake is recommended.
It is important that the nurse recognize and acknowledge the patient’s loss or threatened loss. The patient is educated that it is normal to go through a grieving process. The patient should also be provided with appropriate community referrals for counseling and/or support groups. A patient may be eager to become pregnant again after losing a fetus; however, she should be encouraged to allow her body to rest and recover before attempting another pregnancy and to discuss with her healthcare practitioner when the appropriate time to conceive would be.
CASE
Rihanna is 29 years old and pregnant for the fifth time. Her first pregnancy resulted in birth at 34 weeks’ gestation and produced her only living child. She subsequently had three pregnancy losses at 12 weeks, 14 weeks, and 18 weeks. Rihanna is currently at 12 weeks’ gestation and is at the clinic for her first prenatal checkup. She was seen crying quietly in the waiting room and later states, “My mother-in-law says that if I weren’t such a weak person, I would not keep losing my babies.”
Discussion
Rihanna has had three consecutive pregnancy losses, which indicates that she has a history of recurrent pregnancy losses. Her healthcare practitioner discusses possible causative factors, such as cervical insufficiency or genetic disorders. It is important that Rihanna understand that her behavior did not cause the numerous losses. The nurse caring for Rihanna supports and offers encouragement to her throughout the pregnancy.
(Case study courtesy of Sharon Walker, RN, MSN.)
Ectopic Pregnancy
Ectopic pregnancies occur when the ovum is fertilized by the sperm but implants at a site other than the endometrium of the uterus. Ninety-six percent of ectopic pregnancies occur in the fallopian tubes (Tulandi, 2022a). Other possible implantation sites include the cervix, ovary, or abdominal cavity.
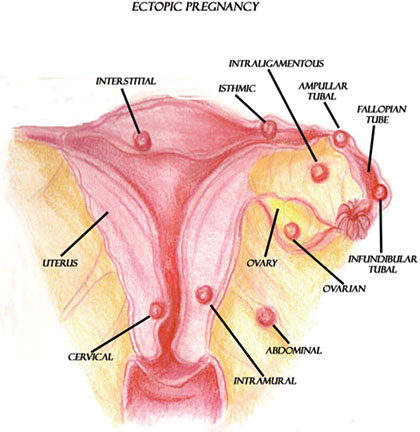
Possible implantation sites for ectopic pregnancies.
(Illustration courtesy of Sim London Jr.)
Ectopic pregnancies are caused by a variety of factors, which include anything that would prevent or slow the fertilized ovum’s journey to the lining of the uterus. More specifically, anything that causes scarring in or blocks the fallopian tubes may cause an ectopic pregnancy.
Patients who are of advanced maternal age or have reproductive system anomalies, a history of tubal surgery, pelvic genital infections, in utero diethylstilbestrol (DES) exposure, intrauterine devices (IUDs), cigarette smoking, in vitro fertilization, or use fertility drugs are at higher risk for having an ectopic pregnancy. The literature also suggests that women who douche regularly have a higher risk of an ectopic pregnancy (Tulandi, 2022b).
SIGNS AND SYMPTOMS
Signs and symptoms of an ectopic pregnancy include vaginal bleeding, lack of menstruation (amenorrhea), and abdominal pain. However, other disease processes (e.g., pregnancy loss) may be responsible for such symptoms. Transvaginal ultrasound and human chorionic gonadotropin (hCG) laboratory testing are necessary to diagnose an ectopic pregnancy.
The outcome of an ectopic pregnancy depends on the location of implantation. The ovum may naturally reabsorb into the body, or the structure supporting the ovum may rupture. If the implantation site is a fallopian tube, the tube may rupture and cause internal hemorrhaging and hypovolemic shock, which is a life-threatening event for the patient.
Signs and symptoms of a ruptured fallopian tube include vaginal bleeding; severe abdominal pain or pelvic, shoulder, or neck pain (as a result of blood leaking out of the fallopian tube and irritating the diaphragm); weakness; dizziness; decreased blood pressure; and increased pulse. It is important to note that many patients experiencing an ectopic pregnancy are asymptomatic prior to tubal rupture.
MEDICAL MANAGEMENT
An ectopic pregnancy implanted in a fallopian tube requires either pharmacologic or surgical management. Pharmacologic management with methotrexate is indicated if the tube is unruptured, the ectopic pregnancy is less than 3–4 cm, there is no fetal cardiac activity, and the patient is stable hemodynamically. Methotrexate is an antimetabolite chemotherapeutic agent that stops cells from dividing and thus stops the gestation. Methotrexate treatment is usually performed on an outpatient basis. Renal and liver function tests should be confirmed before administering methotrexate due to possible toxicity issues (Tulandi, 2022a).
Surgical management includes salpingostomy and salpingectomy. Salpingostomy requires a small linear incision in the tube to remove the pregnancy tissue. This protects the tube for a future pregnancy. A salpingectomy involves the removal of the affected fallopian tube.
NURSING CARE
The nurse caring for a patient experiencing an ectopic pregnancy observes for changes in the patient’s blood pressure and pulse, which could indicate hypovolemic shock resulting from hemorrhage. Regular assessment of vaginal bleeding is also essential. Rh-negative patients require administration of prescribed RhoGAM to prevent alloimmunization. Finally, the nurse is responsible for monitoring and controlling pain levels.
If salpingostomy or salpingectomy is performed, the nurse monitors vital signs, oxygen saturation, intake and output, and laboratory results according to institutional policies. As with all patients experiencing a pregnancy loss, it is important for the nurse to recognize the loss and to provide resources to assist the patient in coping with the emotions that accompany the experience of an ectopic pregnancy.
PATIENT TEACHING
Nurses are responsible for ensuring that the patient is aware of signs and symptoms that require a call to the healthcare practitioner or a return visit to the emergency room following hospital discharge. More specifically, a patient who experiences pain, significant bleeding, or a fever and chills must notify her healthcare practitioner. The nurse should provide the patient with a clear understanding of the normal feelings of anger, sadness, or guilt that may arise following an ectopic pregnancy and that these feelings are part of the grieving process for someone experiencing the loss of a pregnancy.
If laparoscopic surgery was performed, the patient may experience upper abdominal or referred shoulder pain related to carbon dioxide gas inserted into the abdomen during surgery (insufflation). Nurses provide the patient with instructions to ambulate often and to change positions frequently to assist with movement and absorption of this gas.
If methotrexate is used for the treatment of an ectopic pregnancy, the nurse educates the patient about its unpleasant side effects (nausea and vomiting) and informs the patient to avoid vitamins containing folic acid, which can decrease the effectiveness of the medication. The patient should also avoid vaginal intercourse until hCG is undetectable, avoid sun exposure to limit methotrexate dermatitis, and avoid nonsteroidal anti-inflammatory drugs (NSAIDs) (Tulandi, 2022c).
CASE
Cora is a 42-year-old newlywed. She comes into the Women’s Health Clinic complaining of vaginal bleeding and abdominal pain that is completely unlike her usual monthly cramping. She describes her pain as “very sharp” and an “11” on a scale of 0 to 10. Her vital signs are: temperature 98.8 °F, pulse 102 beats/min, respirations 24/min, and blood pressure 102/64 mmHg. She indicates that her blood pressure is “usually 130/90 mmHg.” She is unable to recall the date of her last menstrual period. Additionally, she has almost soaked an entire pad in the last hour.
Cora is very anxious and says, “I’ve never had any real female problems before, except for the little cramping I get on the first day of my period. I shouldn’t be having this difficulty because I keep my female parts very clean by douching weekly.” She sheepishly admits to having had gonorrhea five years ago.
Discussion
Cora is immediately assessed for an ectopic pregnancy. Her risk factors include: advanced maternal age, regular douching, and history of a sexually transmitted infection. She is bleeding heavily and showing evidence of hypovolemia. The priority in this situation is to ensure patient safety by obtaining and sustaining hemodynamic stability. Nursing interventions for Cora include monitoring her vital signs, amount of vaginal bleeding, intake and output, and laboratory results. Cora’s nurses are also involved with administering and teaching about prescribed medications (e.g., RhoGAM, methotrexate) and monitoring for potential side effects.
(Case study courtesy of Sharon Walker, RN, MSN.)
GESTATIONAL TROPHOBLASTIC DISEASE (GTD)
Gestational trophoblastic disease, most commonly the hydatidiform mole or molar pregnancy, occurs when the chorionic villi of the placenta increase as a result of genetic abnormalities. The villi swell, forming fluid-filled sacs, which have the appearance of tiny clusters of grapes within the uterus.
Patients with a GTD exhibit light to heavy bleeding and even hemorrhage. Bleeding can be bright red or watery and brown, appearing similar to prune juice. Anemia may result due to bleeding. Additionally, as a result of the proliferation of tissues and the presence of clotted blood, the uterus may appear larger than expected for gestational age. Despite an enlarged uterus, fetal heart tones and movement are absent. Serum hCG levels are also increased, and patients may experience hyperemesis.
Molar tissues are removed by surgical uterine evacuation. Intravenous oxytocin is usually administered to contract the uterus during suction evacuation to increase uterine tone and decrease blood loss.
Patients are followed for one year after removal of a molar pregnancy to detect choriocarcinoma, or cancer associated with GTD. If serum hCG levels do not return to prepregnancy levels, there is a possibility that choriocarcinoma may be present, and further investigation is necessary. Therefore, it is essential that patients understand the need for follow-up.
Placenta Previa
Placenta previa is the complete or partial covering of the internal os of the cervix by the placenta (see illustration). Placenta previa occurs when the placenta implants in the lower portion of the uterus near the internal cervical os. Previas are classified according to the degree to which they cover the os. Specifically, if the lower border of the placenta is less than 2 cm to the internal cervical os but not covering the os, the placenta is considered low-lying.
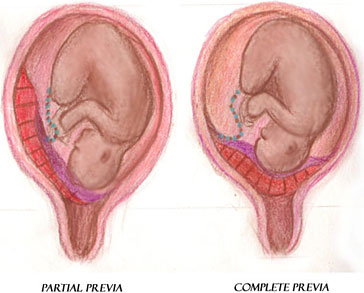
Placenta previa with partial covering of the internal os (left) and placenta previa with complete covering of the internal os (right).
(Illustration courtesy of Sim London Jr.)
As the pregnancy nears term and the cervix dilates, the placenta implanted near or over the internal cervical os is disrupted and bleeding can occur. The bleeding places the patient and fetus at risk. The major factors that place patients at risk for a placenta previa include previous placenta previa, previous cesarean delivery (risk increases with an increasing number of cesarean deliveries), and multiple gestation (Lockwood & Russo-Stieglitz, 2022a).
SIGNS AND SYMPTOMS
The most significantly recognized symptom of placenta previa is painless, bright-red vaginal bleeding or hemorrhage during late pregnancy. However, bleeding may not occur until labor begins. If there is a diagnosis or high suspicion of placenta previa, it is imperative that vaginal examinations be avoided, because stimulation of the placenta may cause hemorrhage. The bleeding as a result of placenta previa could cause the patient to hemorrhage and go into shock, and the fetus could experience hypoxia and possibly death from maternal bleeding.
As a result of the abnormally implanted placenta, the fetus is often in a transverse or breech position, which may be noted during fundal examination.
MEDICAL MANAGEMENT
As previously mentioned, vaginal examination must be avoided if a patient presents with painless, bright-red vaginal bleeding because hemorrhage may occur. A transabdominal ultrasound can be performed to diagnose the previa. It may be followed by a transvaginal ultrasound in order to better visualize the cervix and placenta. Medical management of a placenta previa is largely determined by gestational age, fetal status, amount of bleeding, and type of previa.
Some patients may deliver vaginally if they are near term, the cervix is ripe, the previa is not total, the fetal heart tracing does not show fetal compromise, and there is minimal bleeding. However, if heart tracings indicate fetal compromise, significant bleeding, or hemorrhage, or a complete previa is present, a cesarean section is usually necessary.
NURSING CARE
Nursing care for patients hospitalized with a placenta previa involves close monitoring of bleeding as well as fetal and maternal status. Significant bleeding or hemorrhage should be quantified and reported immediately to the appropriate healthcare provider. Careful monitoring of bleeding is imperative, as vital sign changes may not be initially evident. Regular assessment of fetal heart rate (FHR) and movement is necessary. Heart rate patterns that indicate fetal compromise (i.e., recurrent late or prolonged decelerations, absent or marked FHR variability) should be reported to the healthcare practitioner immediately.
Nonstress testing to evaluate fetal status is performed during bleeding episodes according to medical orders or institutional policy. Patients should be blood-typed and cross-matched in case a blood transfusion is necessary. Blood loss should be quantified. Intravenous access should be maintained for prompt administration of fluids or blood products.
Anti-D-immune globulin (RhoGAM) is given to Rh-negative patients during each bleeding episode to prevent alloimmunization. If bleeding episodes are within three weeks of administration, readministration is not necessary (Lockwood & Russo-Stieglitz, 2022b).
PATIENT TEACHING
Patients with a placenta previa and a history of bleeding should avoid moderate and strenuous exercise, heavy lifting, and standing for prolonged periods, and are encouraged to prohibit vaginal examinations. Patients are advised to avoid any sexual activity that may lead to orgasm, since the uterine contractions that result could provoke bleeding. They are also advised to call their provider promptly if bleeding or labor occurs. If asymptomatic, cesarean section should be scheduled at 36 to 37 weeks (Lockwood & Russo-Stieglitz, 2022b).
Placental Abruption
Placental abruption, often referred to as an abruption or abruptio placentae, is the premature separation of the normally implanted placenta from the uterine wall before delivery of the fetus. It is considered an obstetrical emergency. Bleeding occurs between the uterine wall and the placenta.
Placental abruption is a potentially life-threatening event for the patient and the fetus, depending on the severity of the abruption. Patients with an abruption are at risk for developing hypovolemic shock, disseminated intravascular coagulation (DIC), and possibly death. Since the placenta is the source of oxygenation for the fetus, premature separation of the placenta from the uterine wall can place the fetus at great risk for hypoxia and death.
Placental abruption is classified according to the degree of placental separation and subsequent hemorrhage. An abruption can be partial or complete, with apparent or concealed hemorrhage (see illustrations). An abruption is partial if a section of the placenta separates from the uterine wall but a portion of the placenta remains attached. A complete abruption, the most emergent form, occurs when the entire placenta detaches from the uterine wall. Apparent hemorrhage refers to bleeding that is evident, while a concealed hemorrhage denotes bleeding that is obscured.
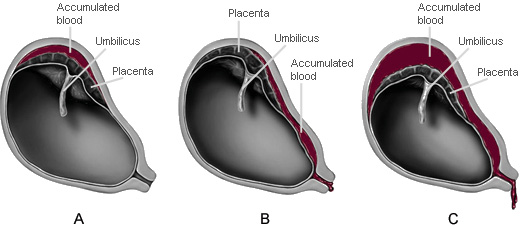
A. Partial placental abruption with concealed hemorrhage
B. Partial placental abruption with apparent hemorrhage
C. Complete placental abruption with apparent hemorrhage
(Illustrations by Jason McAlexander. © Wild Iris Medical Education.)
Aside from abruptions occurring as a result of trauma, the cause of placental abruption is largely unknown. However, there are several factors that place patients at risk for an abruption, including the strongest risk factors of previous abruption, cocaine or other drug abuse, and eclampsia (Ananth & Kinzler, 2022).
SIGNS AND SYMPTOMS
The classic signs and symptoms of placental abruption include an abrupt onset of vaginal bleeding, which may be dark red due to old blood from a concealed abruption; uterine tenderness; and a board-like abdomen. Patients often complain of an aching or dull pain in the abdomen or lower back. Additionally, frequent uterine contractions with poor uterine resting tone (the baseline pressure of the uterus between contractions) are frequently noted.
MEDICAL TREATMENT
Placental abruption is usually diagnosed by abdominal ultrasound in addition to the presenting signs and symptoms. Treatment is based on the degree of placental separation and subsequent hemorrhage as well as the status of the patient and fetus. In the presence of severe abruption and hemorrhage, emergency cesarean section is performed unless delivery is imminent.
NURSING CARE
Although vaginal delivery is preferred to cesarean section for patients who are hemodynamically stable, the nurse must be prepared to deal with the possibility of severe hemorrhage and hypovolemic shock, as well as the resulting fetal distress. Intravenous access with a large-bore catheter is placed to accommodate the administration of fluid and blood products.
It is necessary to monitor carefully the status of the patient and fetus. Frequent vital signs and fetal heart tones, as well as monitoring and documentation of blood loss, is essential. Maternal bleeding may be indicated by falling hemoglobin and hematocrit or abnormal CBC (complete blood count). Abnormal vital signs, bleeding, or fetal heart patterns indicating fetal compromise should be reported immediately to the appropriate healthcare provider. Observation and documentation of the patient’s intake and output and pain and comfort levels are also essential. Patients should be blood-typed and cross-matched in case a blood transfusion is necessary. RhoGAM is indicated for Rh-negative patients. Fetal distress may be indicated by electronic fetal monitoring changes, such as tachycardia followed by bradycardia, absent variability, decelerations, and/or sinusoidal tracing.
Because the potential for patient and fetal injury is high in the presence of placental abruption, it is important to address the emotional needs of the patient. Patients should be kept informed of the status of the fetus, and the nurse should be available and ready to answer any questions that patients or their families may have.
PATIENT TEACHING
Patients are instructed to report bleeding and severe abdominal pain immediately. It is important to inform patients with placental abruption that emergency delivery may be necessary. If a patient must have an emergency cesarean section, the nurse must quickly communicate to the patient and family what will occur before and during the procedure. Nurses should remember that hemorrhage and emergency surgery can be very frightening; therefore, clear and honest information must be given to the patient and family as frequently as possible.
| Assessment | Placenta Previa | Placental Abruption |
|---|---|---|
| Pain | Painless | Uterine tenderness; severe abdominal pain and possibly aching or dull pain in the lower back |
| Bleeding | Bright red | May be concealed; if noted, it is often dark red |
| Uterus | No unusual contractions or irritability | “Board-like” abdomen; uterine irritability with poor resting tone |
| Risk for postpartum hemorrhage | High risk; due to low placement of the placenta, there is limited uterine contraction | High risk due to poor contractility of the uterus following an abruption |
CASE
Rebecca has her first prenatal visit at 30 weeks’ gestation. She is extremely quiet, holds her head down, and stays very close to her husband, speaking in whispers only to him. Rebecca’s husband then repeats her comments and questions to the nurse and clinic staff. Her uterine height and the fetal heart tones are all within normal limits. However, the nurse observes multiple bruises in various stages of healing on the patient’s torso and legs and a moderate amount of dark vaginal blood on her peri-pad. Although Rebecca (through her husband) denies any pain, she is sweating profusely and seems to have abdominal pain.
Discussion
The presence of bruises at various stages of healing and Rebecca’s dependence on her partner to answer for her are possible indications of intimate partner violence. There is also a possibility of placental abruption related to abdominal trauma. The patient has dark red vaginal bleeding and evidence of abdominal pain. It is important for the healthcare practitioner to speak with Rebecca in private to discern the cause of her bruising and possible abuse. In addition, the nurse must ensure the safety of the patient and the fetus.
(Case study courtesy of Sharon Walker, RN, MSN.)