TYPES OF STROKE
The two major categories of stroke—ischemic and hemorrhagic—are diametrically opposite conditions, each resulting from underlying pathophysiologic states. Two other subtypes of stroke are transient ischemic attack (TIA) and cryptogenic stroke.
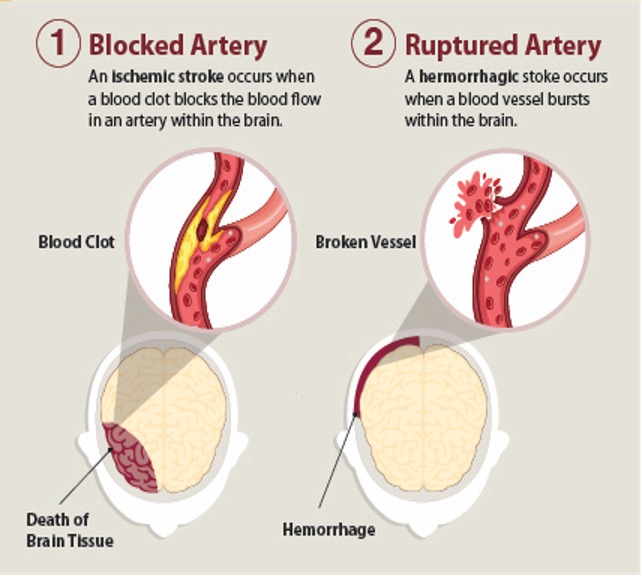
Two primary stroke types: ischemic and hemorrhagic. (Source: CDC.)
Ischemic Stroke
Most strokes (87%) are ischemic. They are characterized by the sudden loss of blood circulation to a specific area of the brain caused by an occlusion of a cerebral artery, resulting in a corresponding loss of neurologic function. Ischemia results in the loss of oxygen and nutrients to the brain cells, and local blood flow is limited to any residual flow in the major arterial source plus the collateral supply, if any (ASA, 2022b).
The etiology of ischemic stroke is due to either a thrombotic or embolic event.
- Thrombotic stroke: Thrombotic strokes are responsible for about half to two thirds of all strokes (LeWine, 2022). Cerebral thromboses are clots that form in the cerebral arterial tree. Blood clots usually form in arteries that are damaged by atherosclerotic plaque but may also be due to arterial dissection or fibromuscular dysplasia, or an inflammatory condition. There are two types of thrombotic stroke: large vessel thrombosis and small artery thrombosis (lacunar infarction).
- Embolic stroke: Cerebral emboli occur due to clots or other debris (such as pieces of plaque) arising from outside the cerebral arterial tree that block arterial access to a particular brain region. A main cause of embolism is atrial fibrillation, and the most common source of the clot is the valves or chambers of the heart. Other less frequent causes include venous, septic, air, or fat emboli.
- Systemic hypoperfusion: This is a more general circulatory problem that manifests itself in the brain and other organs and may be the result of cardiac pump failure or reduced cardiac output related to acute myocardial ischemia, pulmonary embolism, pericardial effusion, or bleeding (ASA, 2022b; Sanchetee, 2021; Hui et al., 2022).
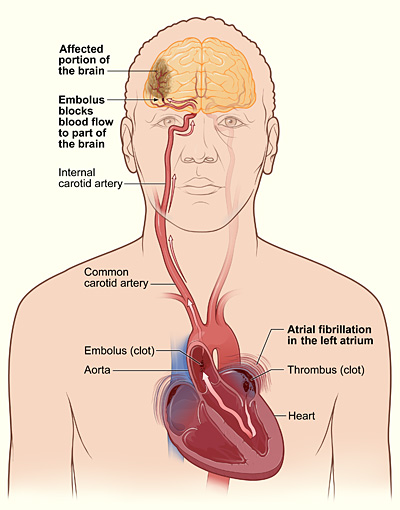
Embolic stroke due to a thrombus formed in the atrium. (Source: NHLBI.)
ANSWERING PATIENT QUESTIONS
Q: What is the difference between a stroke, a brain attack, and a cerebrovascular accident (CVA)?
A: These are three different names for the same thing.
Q: What is a stroke? What are the different types?
A: There are two main types of stroke: ischemic and hemorrhagic.
The most common type of stroke is ischemic. In an ischemic stroke, a brain artery becomes blocked, most commonly by a blood clot. The region of the brain normally supplied by that artery no longer gets enough blood, and that part of the brain becomes starved for oxygen and sugar. Without oxygen and sugar, nerve cells stop working, so the affected region of the brain can no longer perform its particular functions, such as moving an arm or a leg.
A less common type of stroke is hemorrhagic, which means “bleeding.” In a hemorrhagic stroke, an artery is torn, and blood begins to leak out and form a pool in or surrounding the brain. When the blood is leaking out of the artery, it is not carrying sufficient oxygen and sugar to the region that it normally supplies, and the person has the same problems as in an ischemic stroke. In addition, in a hemorrhagic stroke, the pool of blood expands and pushes on the neighboring blood vessels and brain cells. The pressure of the expanding pool of blood causes additional brain damage.
Q: I have heart disease, and my primary care provider said I might have a stroke. How can heart disease affect the brain?
A: Most strokes are caused by clots that become stuck inside arteries in the head and then cut off the supply of blood to the brain.
Both heart disease and strokes can be caused by atherosclerosis. Just as in a stroke, heart attacks and attacks of chest pain (called angina) are often caused by blood clots. Blood clots in the heart usually come from atherosclerosis. Atherosclerosis is a disease that can affect all the large arteries in the body, and some clots formed by atherosclerosis can be swept into the brain. Therefore, if a person has blood clots in their heart, then they also have a chance of getting blood clots elsewhere, such as in their brain.
Another relation between heart disease and strokes has to do with problems in the rhythm of the heartbeat. Irregular heart rhythms can cause blood clots. One particular heart rhythm irregularity, called atrial fibrillation, is notorious for putting a person at risk for a stroke. If you have atrial fibrillation, ask your primary care provider (PCP) how you can reduce your chance of getting a stroke. Also ask your PCP to teach you the warning signs of a stroke.
PATHOPHYSIOLOGY OF ISCHEMIC STROKE
Interruption of blood flow through an intracranial artery leads to deprivation of oxygen and glucose in the supplied vascular territory. This initiates a cascade of events at a cellular level that, if circulation is not reestablished in time, will lead to cell death, mostly through liquefactive necrosis (Sharma, 2022).
Following a stroke, the affected areas of the brain that receive blood flow of less than 10 ml per each 100 grams of tissue per minute are referred to collectively as the core. The cells in the core are presumed to die within minutes of stroke onset. Zones of decreased or marginal perfusion with less than 25 ml per each 100 grams of tissue per minute are collectively called the ischemic penumbra. The tissue in the penumbra can remain viable for several hours because of this marginal tissue perfusion (Jauch, 2022).
ISCHEMIC PENUMBRA PROVIDES EARLY THERAPEUTIC WINDOW
After an ischemic stroke in which the ischemic penumbra has not yet been damaged structurally, permanent structural damage may be prevented if prompt restoration of perfusion in the penumbra can be restored. Collateral and residual blood flow can preserve neurons in the penumbra and border areas for as long as six hours after an ischemic stroke, and within this six-hour window, certain treatments can reduce the amount of damage that is irreversible (Ermine et al., 2021).
Evolution of Ischemic Stroke
The temporal evolution of an ischemic stroke occurs in five stages (see table below).
| Stage | Time frame | Description |
|---|---|---|
| Early hyperacute | 0–6 hours | Growth of the lesion |
| Late hyperacute | 6–24 hours | Swelling develops and intracranial pressure increases |
| Acute | 24 hours–1 week | Extended volumes of critically hypo-perfused cortical tissue |
| Subacute | 1–3 weeks | Swelling starts to subside |
| Chronic | >3 weeks | Residual swelling passes and healing begins |
Microscopically, there is also a temporal neuronal evolution of an ischemic stroke. Immediately following an ischemic stroke, the histological appearance of neuronal tissue begins to change.
- 0–5 minutes: Irreversible neuronal injury occurs.
- 12–24 hours: Red neurons are the first pathological microscopic finding post ischemic stroke. These are indicative of acute neuronal injury and subsequent apoptosis (cell death triggered by normal processes) or necrosis (cell death triggered by external factors). The red color comes from acidophilic cytoplasmic granules of eosinophilic neurons. These neurons can persist in the ischemic penumbra for 2–6 months.
- 24–72 hours: Neuronal cell necrosis and acute inflammatory response are seen.
- 1–3 days: Liquefactive tissue necrosis and neutrophilic infiltration are seen. The brain’s necrotic tissue becomes liquified due to proteolytic enzymes released by microglial cells.
- 3–5 days: Microglia (a macrophage specific to the CNS) become activated around the dying neuron cells to clean cell debris and release mediators of inflammation.
- 1–2 weeks: Gliosis occurs, creating more and larger glial cells that protect and support nerve cells and maintain homeostasis. These new cells can cause scars in the brain that impact how the body functions. Vascular proliferation is also seen. Reactive astrocytes stimulate angiogenesis, which induces vascular proliferation by secreting vascular endothelial growth factor.
- 2 weeks: Glial scars are seen, resulting from a healing process formed to separate and sanction off damaged tissue. Pericytes (cells present along the walls of capillaries) appear to contribute to glial scar formation.
- Over 1 month: Necrotic tissue will be completely removed, and a cystic cavity surrounded by a glial scar will be formed.
(Sharma, 2022: Picmonic, 2022)
CLINICAL PRESENTATION OF ACUTE ISCHEMIC STROKE (AIS)
Ischemic strokes typically give rise to specific (focal) and often painless neurologic symptoms. Onset is abrupt and may progressively evolve over 24–48 hours. Most patients are involved in normal daily activities and notice these common symptoms:
- Sudden numbness or weakness of the face, arm, or leg, especially involving one side of the body
- Sudden confusion or trouble speaking or understanding
- A change in the vision of one or both eyes that occurs suddenly with no known cause
- A quick onset of dizziness, loss of coordination/balance, or other problems walking
- Sudden, severe headache with no known cause
Some patients may also experience a sudden loss of consciousness, fainting or a seizure without a known cause, and vomiting or fever that occurs within minutes or hours that cannot be explained by another cause. In large vessel ischemic stroke, headache may occur prior to, during, or following stroke onset.
The effects of an AIS may cause additional symptoms in women, including:
- Face, arm, or leg pain
- Hiccups or nausea
- Chest pain or palpitations
- Shortness of breath
(Beaumont, 2022a; Cedars Sinai, 2022)
ISCHEMIC STROKE SYNDROMES
Specific neurologic functions are dependent on specialized brain regions, with each artery primarily supplying a particular region. Thus, occlusion in particular branches of the major cerebral arteries produce characteristic stroke syndromes, which are symptom complexes caused by impaired blood supply to specific areas of the brain. These syndromes help clinicians to infer which brain areas have been damaged in a specific patient’s stroke.
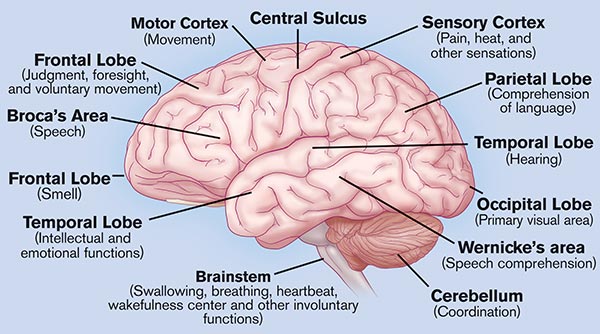
Brain regions and associated neurologic functions. (Source: Activase Image Library.)
Anterior Cerebral Artery (ACA) Stroke Syndrome
The anterior cerebral artery provides blood to the medial portion of the brain: frontal, prefrontal, primary motor, primary sensory, and supplemental motor cortices. The clinical features of this syndrome include:
- Contralateral hemiplegia (lower extremity greater than upper extremity/face)
- Contralateral sensory loss
- Urinary incontinence
- Fecal incontinence
- Abulia (apathy)
- Akinetic mutism (a rare condition of pathologically slowed or nearly absent bodily movement accompanied by loss of speech)
- Transcortical motor aphasia (nonfluent speech, comprehension intact, and can repeat phrases)
- Anosmia (loss of smell) related to olfactory bulb infarction
- Alien hand syndrome (in which patient thinks the hand is not part of their body and that they have no control over its movement)
- Gait apraxia (disequilibrium and inability to lift the feet off the floor)
- Dysarthria (inability to control muscles used in speech)
- Aphasia (inability to understand or express speech)
(Yartsey, 2022; Strokenetwork, 2022)
Internal Carotid Artery Syndrome
The internal carotid arteries are part of the anterior circulation supplying blood to the forebrain. The clinical features of this syndrome include:
- Amaurosis fugax (transient monocular or binocular visual loss)
- Affects circulation to the middle cerebral artery, anterior cerebral artery, and the posterior cerebral artery resulting in the presentation of the middle cereberal artety (MCA) syndrome, anterior cerebral artery (ACA) syndrome, and posterior cerebral artery (PCA) syndrome
(Murphy, 2021)
Middle Cerebral Artery (MCA) Stroke Syndrome
Two thirds of ischemic strokes occur in the MCA because of the size of the territory and the direct flow from internal carotid artery into the middle cerebral artery. Clinical presentation will depend on the extent of the infarct and hemispheric dominance.
If the infarct occurs in the left hemisphere (i.e., dominant), the resulting signs and symptoms can include:
- Right motor and sensory deficit (face and arm/leg/foot)
- Complete hemiplegia if internal capsule involved
- Right homonymous hemianopia (a visual field loss deficit in the same halves of the visual field of each eye)
- Dysarthria
- Aphasia, fluent and nonfluent
- Alexia (inability to read)
- Agraphia (inability to write)
- Acalculia (inability to do simple arithmetic)
- Apraxia (inability to perform a familiar movement on command, even though the command is understood and there is willingness to perform the movement)
If the infarct occurs in the right hemisphere (i.e., nondominant), the following signs and symptoms can occur:
- Contralateral hemiparesis
- Contralateral sensory loss
- Left hemianopsia (blindness or reduced vision in half the visual field)
- Dysarthria
- Hemispatial inattention (contralateral neglect of the left side of the environment)
- Anosognosia (lack of insight)
- Asomatognosia (the impression that one’s own body has ceased to exist)
- Loss of prosody of speech (intonation, stress pattern, loudness variations, pausing and rhythm)
- Flat affect
(Yartsey, 2022; Strokenetwork, 2022)
Posterior Cerebral Artery (PCA) Stroke Syndrome
The PCA supplies blood to multiple brain regions: occipital lobe, inferomedial temporal lobe, a large portion of the thalamus, upper brainstem, and midbrain. Clinical features for each region include:
Occipital:
- Contralateral homonymous hemianopia (a visual field defect involving either the two right or two left halves of the visual fields of both eyes)
- Visual disturbances, such as color anomia
- Hallucinations
- Sensory loss
- Strabismus (eye misalignment)
- Ptosis (droopy eyelid)
- Mydriasis (enlarged pupil) with abnormal reaction to light
- Choreoathetosis (involuntary movements with twisting and writhing)
- Spontaneous pain
- Cranial nerve III palsy (impaired eye movements and pupillary reaction to light)
- Motor deficit
- Cortical blindness (bilateral lesions)
- Anosognosia (unawareness or denial of blindness)
Medial temporal lobe:
- Deficits in long- and short-term memory
- Behavior alterations (agitation, anger, paranoia)
Thalamus:
- Contralateral sensory loss
- Aphasia (if dominant side involvement)
- Executive dysfunction
- Decreased level of consciousness
- Memory impairment
(Strokenetwork, 2022)
Brainstem Stroke Syndrome
There are many brainstem stroke syndromes. Brainstem infarcts affect the midbrain, pons, and medulla oblongata, which can cause a varied range of symptoms. Early diagnosis is a must, as brainstem infarction is associated with high mortality and morbidity. Some of the clinical features seen are:
- Crossed sensory and motor findings (e.g., ipsilateral face and contralateral body numbness)
- Gaze-evoked nystagmus (rapid involvement eye movements)
- Ataxia and vertigo
- Limb dysmetria (lack of coordination of movement typified by the undershoot or overshoot of intended position with hand, arm, leg, or eye)
- Diplopia and eye movement abnormalities
- Dysarthria
- Dysphagia
- Tongue deviation
- Deafness (very rare)
- Locked-in syndrome
(Strokenetwork, 2022)
Cerebellar Stroke Syndrome
Cerebellar strokes are rare and, if left untreated, can be life-threatening. Cerebellar strokes can cause:
- Ataxia
- Nystagmus
- Vertigo
- Nausea, vomiting
- Dysarthria
- Headache
- Rapid deterioration in consciousness
(Strokenetwork, 2022)
Lacunar Stroke Syndrome
Lacunar stroke is common and most of the time asymptomatic but can cause significant morbidity and mortality. It is due to occlusion of the small branches of the cerebral vessels from the circle of Willis. Characteristic pattern of lacunar strokes may include:
- Pure motor hemiparesis
- Absence or abnormal sensation of contralateral face, arm, and leg
- Ataxic hemiparesis
- Clumsy hand–dysarthria
- Contralateral facial weakness with dysarthria and dysphagia
- Contralateral hand weakness, ataxia, and sometimes weakness in the arm or leg
(Yartsey, 2022; Strokenetwork, 2022)
Vertebral Artery Stroke Syndrome
These strokes are relatively uncommon but are a disproportionate cause of morbidity and mortality due to discrete symptoms that resemble nonstroke medical conditions. The most common symptoms experienced by patients include:
- Disequilibrium
- Vertigo
- Diplopia
- Cortical blindness (total or partial loss of vision in a normal-appearing eye)
- Alternating paresthesia
- Tinnitus
- Dysphasia
- Dysarthria
- Quadriplegia
- Drop attacks (sudden fall without warning)
- Ataxia
- Perioral numbness
- Bilateral sensorimotor deficit
- Respiratory dysfunction
- Consciousness impairment/coma
Other signs and symptoms may include:
- Unilateral limb weakness
- Dysarthria
- Dysphagia
- Headache
- Nausea and vomiting
- Gait ataxia
- Nystagmus
- Perioral numbness
(Morasch, 2021)
Basilar Artery Stroke Syndrome
Patients with acute occlusion of the basilar artery will present with sudden and dramatic neurologic impairment, the exact characteristics dependent upon the site of occlusion:
- Sudden death/sudden loss of consciousness
- Visual and oculomotor deficits
- Behavioral abnormalities
- Somnolence, hallucinations, and dream-like behavior
- Locked-in syndrome
- Quadriparesis
- Respiratory muscle paralysis
- Preserved consciousness
- Preserved ocular movements
(Glick, 2021; Ikram & Zafar, 2022)
CRYPTOGENIC STROKE
Cryptogenic strokes comprise 25%–40% of ischemic strokes. Cryptogenic strokes are those in which a comprehensive evaluation cannot define the cause. Most cryptogenic strokes produce symptoms similar to those of strokes known to be caused by emboli; nonetheless, the strokes are labeled cryptogenic if available tests cannot document the specific cause (Prabhakaran & Elkind, 2022).
Transient Ischemic Attack (TIA)
A transient ischemic attack, sometimes called a mini-stroke, is a warning sign of a future stroke. It is different from the major types of stroke because blood flow to the brain is blocked for only a short time—usually no more than five minutes. For this reason, a TIA is often dismissed and not taken seriously.
A TIA is a brief interruption of blood flow, most often caused by thrombosis, to part of the brain, spinal cord, or retinas. TIA may cause temporary stroke-like symptoms but does not damage brain cells or cause permanent disability. There is brief neurologic dysfunction, with clinical symptoms typically lasting less than one hour and without evidence of acute infarction.
More than one third of people who have a TIA and don’t get treatment have a major stroke within one year. As many as 10%–15% of people will have a major stroke within three months of a TIA (CDC, 2022b; Rost & Fay, 2022).
CLINICAL PRESENTATION OF TIA
A person experiencing a transient ischemic attack may have one or more of the following signs or symptoms:
- Weakness or numbness in the arms and/or legs, usually on one side of the body
- Dysphasia
- Dysarthria
- Dizziness
- Sudden vision changes
- Paresthesias (tingling)
- Abnormal taste and/or smells
- Confusion
- Sudden trouble walking, loss of balance or coordination
- Altered consciousness and loss of consciousness
(Panuganti et al., 2022)
Hemorrhagic Stroke
Intracranial bleeding caused by a blood vessel within the cranium that has leaked or ruptured is called a hemorrhagic stroke. Hemorrhagic strokes are less common than ischemic strokes, making up about 13% of all strokes. Risk of death related to each bleed is 10%–15%, and the chance of permanent brain damage is 20%–30%. There are two types of hemorrhagic strokes:
- Intracerebral hemorrhage (ICH), the most common type, occurs when a blood vessel within the brain ruptures.
- Subarachnoid hemorrhage (SAH) refers to bleeding in the subarachnoid space, the area between the brain and the meninges that cover it.
(ASA, 2022b)
PATHOPHYSIOLOGY OF HEMORRHAGIC STROKE
An intracranial hemorrhage is most commonly the result of hypertension. Bleeding occurs suddenly and rapidly. There are usually no warning signs, and bleeding can be severe enough to cause coma or death. Subarachnoid hemorrhage is often due to an aneurysm or an arteriovenous malformation (AVM) but can also be caused by trauma.
An aneurysm is a ballooning of a weakened region of a blood vessel. If untreated, it continues to weaken until it ruptures and bleeds into the brain. Berry (saccular) aneurysms are the most common type of intracranial aneurysms (90%), and 85% off these are located in the circle of Willis.
Ruptured brain aneurysms are fatal in about 50% of cases, and approximately 15% of people with a ruptured aneurysm die before reaching the hospital. Of those who survive, about 66% suffer some permanent neurologic deficit. Brain aneurysms are most prevalent in people ages 35 to 60 but can occur in children as well (BAF, 2022).
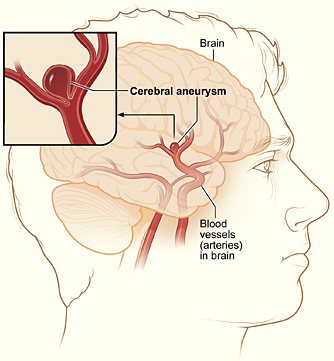
A typical location of a cerebral aneurysm in the arteries that supply blood to the brain. (Source: NIH.)
Arteriovenous malformations (AVMs) are dilated tangled blood vessels in which the arterial blood flows directly into the venous system, bypassing the capillary bed within the brain tissue or on its surface. Brain AVMs are usually congenital but not hereditary. AVMs do not grow or change much, although the vessels involved may dilate over time and eventually burst. More than 50% of patients with an AVM have an intracranial hemorrhage. Risk of death related to each bleed is 10%–15%, and the chance of permanent brain damage is 20%–30% (ASA, 2022d).

Cranial arteriovenous malformation. (Source: © Michel Royon / Wikimedia Commons.)
There are different mechanisms of brain injury in intracranial hemorrhage, including:
- Primary mechanical injury to the brain parenchyma occurs via hematoma expansion and perilesional edema. This can increase intracranial pressure, which can cause reduced cerebral perfusion and ischemic injury. In very large ICH, cerebral herniation can occur, compressing the brainstem and often causing secondary hemorrhage in the midbrain and pons.
- Secondary brain injury is caused by the breakdown of the blood-brain-barrier after the initial hemorrhage, including excitotoxic and inflammatory processes.
(Rordorf & McDonald, 2022)
ANSWERING PATIENT QUESTIONS
Q: Can a stroke be stopped?
A: A stroke is the set of symptoms that follow when a brain artery is blocked or bleeding. The brain can often recover if the cause of the stroke can be reversed and fresh blood can be gotten to the blood-starved areas soon enough.
When the underlying problem is a blocked artery, the stroke symptoms will sometimes lessen or even disappear if the obstructing clot is removed or dissolved quickly enough. In the case of bleeding arteries, these will sometimes stop bleeding on their own, and sometimes they can be coaxed to slow down or stop. If the bleeding can be stopped, the stroke symptoms will sometimes lessen.
CLINICAL PRESENTATION OF HEMORRHAGIC STROKE
Symptoms of intracerebral hemorrhage often begin with a sudden headache occurring during activity. However, headache may be mild or absent in the older adult. Loss of consciousness is common, often within seconds or a few minutes. Nausea, vomiting, delirium, and focal or generalized seizures are common.
Neurologic deficits usually are sudden and progressive. Large hemorrhages, when occurring in the hemispheres, cause hemiparesis; when occurring in the posterior fossa, they cause cerebellar or brainstem deficits, such as stertorous (low-pitched, nonmusical) breathing, pinpoint pupils, coma, conjugate eye deviation, or ophthalmoplegia (extraocular muscle paralysis).
A large intracerebral hemorrhage is fatal within a few days in approximately half of patients. In those who survive, consciousness returns and neurologic deficits gradually diminish to different degrees as the blood is resorbed. Some patients may have only a few neurologic deficits due to the fact that hemorrhage is less destructive to the brain tissue than an infarct.
Small hemorrhages may result in focal deficits with no impairment of consciousness and with minimal or no headache or nausea, and they may mimic ischemic stroke (Chong, 2020a).
Symptoms of subarachnoid hemorrhage begin abruptly with a severe headache (often referred to as a thunderclap headache or WHOML, “worst headache of my life”), which peaks within seconds. Loss of consciousness may follow, usually immediately, but sometimes not for several hours.
Severe neurologic deficits may develop and become irreversible within minutes or a few hours. Sensorium may be impaired, and patients may become restless. Seizures are possible.
Usually, the neck is not stiff initially, unless the cerebellar tonsils herniate. However, within 24 hours, chemical meningitis causes moderate to marked meningismus, vomiting, and sometimes bilateral extensor plantar responses. Heart or respiratory rate is often abnormal.
Fever, continued headaches, and confusion are common during the first 5–10 days. Secondary hydrocephalus may cause headache, obtundation, and motor deficits that persist for weeks (Chong, 2020b).