WHAT IS A STROKE?
What is a stroke and how does it happen? For many, a stroke happens suddenly, without any warning, and because the brain controls everything the body does, it can affect how the person moves, feels, thinks, and communicates. Any stroke can be life changing, and it can happen to anyone of any age. The experience of stroke is different for everyone, but some effects are more common than others.
Risk Factors for Stroke
Stroke risk factors have been categorized as either nonmodifiable or modifiable.
NONMODIFIABLE RISK FACTORS
- Age: The incidence of stroke increases with age for both males and females.
- Gender: Women have more strokes than men, and stroke kills more women than men. Factors increasing risk include pregnancy, history of preeclampsia/eclampsia or gestational diabetes, oral contraceptive use, and postmenopausal hormone therapy.
- Race/ethnicity: Disparities among racial and ethnic groups are well-documented (see above).
- Genetics: Family history of stroke in a parent, grandparent, sister, or brother, especially before reaching age 65, increases stroke risk. Some strokes are also caused by genetic disorders such as CADASIL (cerebral autosomal dominant arteriopathy with sub-cortical infarcts and leukoencephalopathy), which occurs when thickening of blood vessel walls blocks the flow of blood to the brain.
- Fibromuscular dysplasia: This medical disorder involves fibrous tissue growth in artery walls, which causes them to narrow.
- Brain aneurysms or arteriovenous malformations (AVMs): Aneurysms are bulges in an artery that can stretch and burst, and AVMs are tangles of faulty arteries and veins that can rupture.
- Viral infections or conditions that cause inflammation: Examples may include lupus, rheumatoid arthritis, and COVID-19, which damage the heart muscle and causes arrhythmias.
- Personal past history of stroke, transient ischemic attack (TIA), or heart attack: A TIA is a brief episode of stroke-like symptoms (lasting from a few minutes to 24 hours but with no permanent damage or disability); it increases the risk of stroke by 10 times.
(AHA, 2021a; NHLBI, 2022)
MODIFIABLE RISK FACTORS
- Hypertension: Elevated blood pressure is the leading cause of stroke and the most important controllable risk factor for stroke.
- Diabetes: While treatable, diabetes increases the risk of stroke.
- Cigarette smoking: Smoking is a major risk factor. Nicotine and carbon monoxide damage the cardiovascular system. Use of birth control pills combined with cigarette smoking can greatly increase the risk. Secondhand smoke has also been identified as an independent risk factor. Smoking may double stroke risk for African Americans.
- Cardiac causes: Atrial fibrillation and atrial cardiopathy are associated with cardioembolic strokes. Atrial fibrillation increases the risks fivefold. Sleep apnea can be linked to atrial fibrillation and is also associated with increased stroke risk.
- Dyslipidemia: High total and LDH cholesterol are risk factors for stroke. HDL levels influence development of hemorrhagic but not infarct stroke. Low HDL cholesterol is protective in hemorrhagic stroke.
- Sedentary behavior: The relationship between physical activity and stroke may be due to its association with decreased blood pressure, reduction in diabetes mellitus, and reduction in excess body weight.
- Diet/nutrition: Diet influences the risks of stroke and other stroke risk factors, including diabetes mellitus, hypertension, and dyslipidemia. Some components are well known, such as salt intake (increased hypertension) and potassium intake (associated with decreased stroke risk).
- Obesity/waist-to-hip ratio: Obesity is related to other stroke risk factors such as hypertension and diabetes mellitus. The major contributor to risk is waist-to-hip ratio rather than overall increased weight as indicated by body mass index.
- Medications: Certain drugs have been shown to increase risk for stroke, especially when used in combination with other risk factors for stroke. These may include anticoagulants and thrombolytic agents, which increase the risk for bleeding.
- Polluted air: Increasing evidence suggests that living or working in areas with air pollution is an emerging risk factor for stroke. Air pollution is now estimated to be responsible for 15% of all stroke-associated deaths.
- Alcohol consumption: The relationship of alcohol to stroke risk depends on the stroke type. Alcohol consumption has a more direct linear relationship with hemorrhagic stroke, and even consuming small amounts of alcohol seem to increase risk of hemorrhages. Heavy drinking is associated with an increased risk of ischemic stroke.
- Other unhealthy lifestyle habits: Getting too much sleep (more than 9 hours) and using illegal drugs (such as cocaine) are associated with increased risk of stroke.
- Infections: Data suggest that chronic exposure to common bacterial and viral infections is a risk factor for stroke and may act as a trigger for stroke. Research has found that the risk of stroke increased after respiratory tract infection but was reduced after vaccination against influenza, pneumococcal infection, and tetanus.
- Genetics: Although most often considered a nonmodifiable risk factor, genetic therapies may change this in the future. Some may be modifiable because environmental factors may interact with genetic mutation, e.g., a person predisposed to diabetes or hypertension could reduce risk through lifestyle modifications. Some may already be modifiable, if not curable, e.g., those with sickle cell anemia can be treated with exchange transfusions to reduce stroke risk.
- Other medical conditions: These may include bleeding disorders, high red blood cell count, sleep apnea, kidney disease, or migraine headaches with aura.
(NHLBI, 2022; Verhoeven et al., 2021)
ANSWERING PATIENT QUESTIONS
Q: My mother died of a stroke. Am I likely to have a stroke, too? What about my children?
A: People whose parents, grandparents, brothers, or sisters had a stroke have a higher risk of stroke themselves. It is therefore of great importance to reduce your chances of having a stroke and thus protect your children against stroke in the future. The following lifestyle measures can help to reduce the risk of stroke.
- Keep your blood pressure in a healthy range. High blood pressure can cause a stroke. People can have high blood pressure without knowing it, so get your blood pressure checked. If you have high blood pressure, follow your healthcare provider’s recommendations.
- Stop smoking. Smokers have a greater risk of having a stroke, and smokers who are also taking birth control pills have an even higher risk. Ask your provider to suggest a stop-smoking plan.
- Control your diabetes. People with diabetes have a higher risk of having a stroke. Follow your provider’s recommendations for controlling your blood sugar levels.
- Keep your cholesterol level low. High blood cholesterol makes a person more likely to develop atherosclerosis, and atherosclerosis is a major cause of strokes. Get your cholesterol level checked. If your cholesterol levels are unhealthy, follow your provider’s recommendations for your diet and take any medications that are prescribed.
- Keep your weight low. Obesity is another condition that will increase your risk of developing a stroke. Losing weight is difficult, so ask your provider for help in making a realistic weight loss plan.
- Stay active. Regular exercise lowers your risk of developing a stroke.
Stroke Triggers
Although there is a good understanding of the major stroke risk factors listed above, what triggers a stroke to occur at a particular point in time remains to be understood. A new area of investigation in stroke epidemiology involves the determination of such stroke triggers. At this time, they may include:
- Infection, particularly of the urinary tract, could trigger a stroke.
- Acute anger or emotional upset is associated with the onset of ischemic stroke and intracranial hemorrhage.
- Heavy physical exertion has been found to be associated with intracranial hemorrhages.
(Wegener, 2021; AHA, 2019)
PATHOLOGIES UNDERLYING STROKES
The primary pathologies underlying stroke are heart or blood vessel diseases, and the secondary manifestations in the brain are the result of one or more of these underlying diseases or risk factors.
Heart conditions may include:
- Atrial arrhythmias (fibrillation, flutter, paroxysmal atrial fibrillation)
- Rheumatic mitral or aortic valve disease
- Prosthetic and mechanical heart valves
- Atrial or ventricular thrombus
- Sinus node dysfunction
- Recent myocardial infarction (within one month)
- Congestive heart failure
- Cardiomyopathy
- Fibrous nonbacterial endocarditis in persons with systemic lupus
- Infective endocarditis
- Papillary fibroelastoma
- Left atrial myxoma
- Coronary artery bypass graft surgery
Blood vessel diseases may include:
- Atherosclerosis
- Hypertension
- Essential thrombocytosis
- Heparin-induced thrombocytopenia
- Noninflammatory blood vessel disorders
- Fibromuscular dysplasia
- Vasospasm after subarachnoid hemorrhage
- Reversible cerebral vasoconstriction syndromes
- Radiation-induced vasculopathy
- Moyamoya disease
- Fabry disease
- Inflammatory blood vessel disorders
- Isolated angiitis of the CNS
- Temporal (giant cell) arteritis
- Cerebral vasculitis related to infection, toxins, or neoplasms
- Hematological disorders
- Inherited and acquired blood clotting disorders
- Prothrombotic disorders
- Polycythemia vera
- Genetic mutations causing disorders of the coagulation system
- Antiphospholipid antibody syndrome
- Sickle cell disease
- Hyperhomocysteinemia
- Thrombotic thrombocytopenic purpura (TTP)
Other pathologies may include:
- Migraine-related stroke
- Cerebral venous thrombosis
(AHA, 2021b; Caplan, 2022a)
Effects of a Stroke
A stroke can have profound effects on the body as well as the mind and emotions. The effects of a stroke depend on several factors, including the location of the obstruction or hemorrhage and how much brain tissue has been affected.
Because one side of the brain controls the opposite side of the body, a stroke affecting one side of the brain will cause neurologic complications on the opposite side of the body. A stroke occurring in the left side of the brain will result in some or all of the following:
- Weakness, numbness, stiffness, or paralysis on the right side of the body
- Speech/language problems (aphasia, also called dysphasia)
- Slow, cautious behavioral style
- Cognitive changes (memory loss)
A stroke occurring in the right side of the brain will result in some or all of the following:
- Weakness, numbness, stiffness, or paralysis on the left side of the body
- Vision problems
- Quick, inquisitive behavioral style
- Cognitive changes (memory loss)
When a stroke occurs in the brainstem, depending on how severe the injury is, both sides of the body may be affected, and the person may be left in what is referred to as a “locked-in” state. When this occurs, the patient is able to think and is cognitively intact, but there is paralysis of all movements except vertical gaze and eyelid opening. These individuals are able to communicate with eye movements.
Damage to the brain following a stroke can result in many cognitive changes, such as the following types of memory loss:
- Memory of names, stories, and information having to do with language (verbal)
- Memory of shapes, faces, routes, and things seen (visual)
- Memory for skills or trouble learning new things (information)
Along with losing memory following a stroke, a person may develop vascular dementia, which causes problems with reasoning, planning, judgment, or other thought processes.
It is common for emotional and behavioral changes to occur as a result of a stroke. A stroke can impact mood and outlook. Mood disorders such as depression and anxiety are common, with depression affecting between one third and two thirds of stroke survivors.
Pseudobulbar affect (PBA) is a neurologic condition that can be caused by a stroke. It is also known as emotional lability, reflex crying, and involuntary emotional expression disorder, among other names. In PBA, there is a disconnect between the frontal lobe (which controls emotions) and the cerebellum and brainstem (where reflexes are mediated). The effects are uncontrollable and can occur without an emotional trigger. PBA is characterized by a mismatch between feelings and expression, such as laughing at a funeral or crying at something that is funny (ASA, 2022a).
ANATOMY AND PHYSIOLOGY OF CEREBRAL CIRCULATION
In order to function normally, the brain depends on receiving adequate oxygen and nutrients through a network of blood vessels. Two major sets of vessels supply blood to the brain. The anterior circulation of the brain is supplied by the right and left common carotid arteries, and the posterior portion of the brain is supplied by the right and left vertebral arteries. Every minute, about 600–700 ml of blood flow through the carotid arteries and their branches, and 100–200 ml flow through the vertebral-basilar system.
The right common carotid artery originates from the bifurcation of the brachiocephalic trunk, while the left common carotid artery originates directly from the aortic arch. Each then branches to form the external and internal carotid arteries. The external carotid arteries supply blood to the face and scalp, and the internal carotid arteries supply blood to most of the anterior portion of the cerebrum.
The vertebral arteries arise from the subclavian arteries and run alongside the medulla, giving rise to branches that supply the cervical spinal cord as well as the brainstem. They end by fusing to form the basilar artery. The vertebra-basilar arteries supply the posterior two fifths of the cerebrum, part of the cerebellum, and the brainstem.
The anterior and posterior circulations communicate through a circular anastomosis of arteries called the circle of Willis, which is located at the base of the brain and serves as an effective collateral circulation, protecting against ischemia in the event of vessel disease or damage in one or more areas (UMass Chan Medical School, 2022).
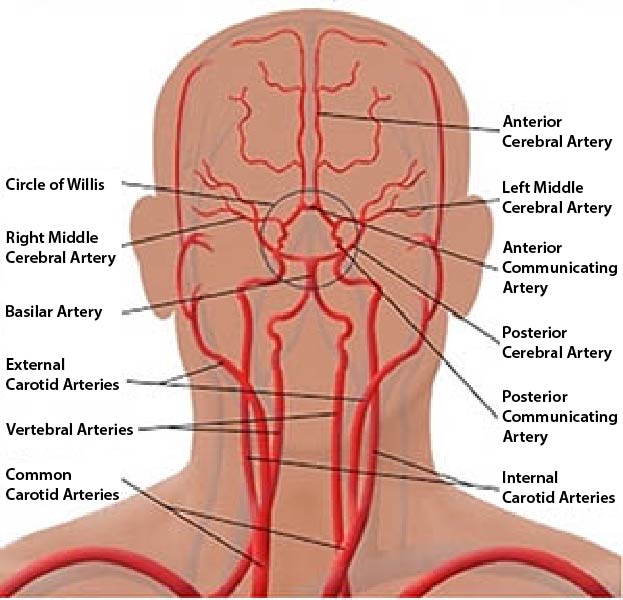
Cerebral vascular system. (Source: Bruno Bordoni, Creative Commons Attribution 4.0 International License.)