EPIDEMIOLOGY
- Globally, 1 in 4 adults over the age of 25 will have a stroke in their lifetime. 13.7 million people worldwide will have their first stroke this year, and 5.5 million people will die as a result.
- In 2020, there were 7.08 million deaths attributable to cerebrovascular disease worldwide (3.48 million from ischemic stroke, 3.25 million from intracerebral hemorrhage, and 0.35 million from subarachnoid hemorrhage).
- Every 40 seconds, someone has a stroke in the United States, totaling more than 795,000 people. About 610,000 of these are first or new strokes, and about 185,000 (nearly 1 in 4) are in people who have had a previous stroke.
- Every 3.5 minutes, someone dies of stroke in the United States. In 2019, stroke ranked number 5 among all causes of death in the United States, with 150,005 deaths, or approximately 1 of every 19 deaths. In 2020, 1 in 6 deaths from cardiovascular disease was due to stroke.
(CDC, 2022a; AHA, 2022a; WSO, 2022)
By Age
Stroke risk increases with age but can occur at any age. Nearly 75% of all strokes occur in people over the age of 65, and the risk of having a stroke more than doubles each decade after the age of 55.
Older people are not the only ones who have strokes. Although it is more common among older people, a stroke can happen to anyone at any time, including teenagers, children, newborns, and unborn babies. Every year about 70,000 Americans under the age of 45 have strokes. About 10%–15% of strokes occur in children and adults under age 45, and that number is rising.
The risk of stroke in children is greater in the first year of life and during the periods right before and right after birth. The cause of most of these perinatal strokes remains unknown. Warning signs are often missed in children because there is a lack of awareness that strokes can happen in this age group (AHA, 2022b; Sutter Health, 2022).
By Gender
Women face a disproportionate burden of stroke mortality and disability. Young women have been found to have a much higher risk of stroke when compared to men. However, this risk reverses as age increases and equalizes at ages above 80 years. Stroke is the third leading cause of death for women and the fifth leading cause of death for men in the United States. Among women, Black women have the highest prevalence of stroke.
Unique risk factors for women include:
- Past oral contraceptive use
- Increased blood pressure and stress on the heart during a normal pregnancy
- Preeclampsia, which doubles the risk of stroke later in life
- Hormone replacement therapy (HRT)
- Migraine headaches with aura (more common in women), which increases risk for stroke 2.5 times
- Atrial fibrillation, which increases the risk of stroke by 20% among women over age 75
(AHA, 2022c)
By Race and Ethnicity
Black people have nearly twice the risk of a first stroke as White people. Strokes among African Americans tend to occur earlier in life, and these individuals are more likely to become disabled from a stroke. Research indicates over two thirds of Black Americans have at least one risk factor for stroke, which can include:
- Hypertension (present in over 50% of Black adults)
- High prevalence of overweight or obesity (present in almost 70% of Black men and 80% of Black women)
- High prevalence of diabetes
- High sodium intake (African Americans may have a gene that greatly increases sensitivity to salt and its effects)
- Prevalence of high levels of LDL (“bad”) cholesterol
- Sickle cell anemia (the most common genetic disorder among African Americans)
Hispanic Americans and American Indian/Alaska Natives are also at greater risk than White people for having a stroke but are at less risk than Black people. The rate of stroke at younger ages is higher in Hispanics than in the rest of the population.
Stroke mortality rates are higher in Black Americans, American Indians, Alaska Natives, Hispanics, Native Hawaiians, and other Pacific Islanders, compared with White Americans. Although stroke death rates have declined over the decades among all other races/ethnicities, Hispanics have seen an increase.
(NIH, 2022; Levine et al., 2020; ASA, 2019)
By Geographic Location
The southeastern United States is often referred to as the “stroke belt” because of its higher stroke incidence and mortality rate. This area includes a higher proportion of rural residents relative to other regions, and nationally, residents of rural regions have a higher stroke incidence compared with those living in more urban areas.
Data suggest that contributors to the higher incidence of stroke in this region may include a larger proportion of Black people and of people with a higher prevalence of traditional stroke risk factors, a higher rate of inflammation and infection, and lower socioeconomic status. Environmental exposures and lifestyle choices are thought to play a lesser role. While substantial progress has been made in gaining an understanding of the contributors to the stroke belt, much work remains to understand this disparity (Howard & Howard, 2020).
The 10 states with the highest mortality rate for stroke in 2019 are:
- Mississippi
- Alabama
- Louisiana
- Delaware
- South Carolina
- Tennessee
- Georgia
- Ohio
- Arkansas
- North Carolina
Pockets of high-rate counties also are found in:
- West Virginia
- Kentucky
- Oklahoma
- Virginia
- Texas
- Alaska
- Missouri
- Michigan
- Georgia
- Delaware
- Maryland
(Statista, 2022)
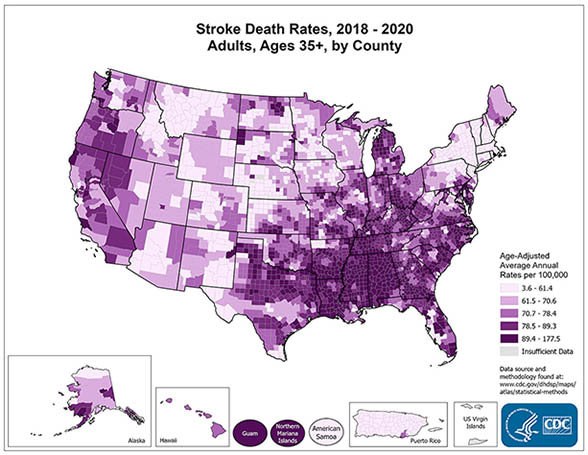
(Source: National Center for Chronic Disease Prevention and Health Promotion.)