Obesity in America
Management and Treatment in Children, Adolescents, and Adults
CONTACT HOURS: 9
Copyright © 2022 Wild Iris Medical Education, Inc. All Rights Reserved.
LEARNING OUTCOME AND OBJECTIVES: Upon completion of this course, you will have increased your knowledge about obesity, including its prevalence, consequences, contributing factors, interventions, and approaches to prevention and treatment. Specific learning objectives to address potential knowledge gaps include:
- Describe the prevalence and impact of overweight and obesity in U.S. adults, children, and adolescents.
- Examine the pathogenesis and etiology of overweight and obesity.
- Discuss the comorbidities and consequences of obesity.
- Explain the psychosocial effects of stigma and weight bias.
- Describe components of assessment for overweight or obesity.
- Summarize strategies for management and treatment of overweight and obesity in adults, children, and adolescents.
- Discuss considerations in caring for the bariatric patient.
- Outline ways to prevent overweight and obesity in all age groups.
TABLE OF CONTENTS
- Introduction
- What Causes Obesity?
- Comorbities and Consequences of Obesity
- Assessing for Overweight and Obesity
- Management and Treatment of Obesity in Adults
- Management and Treatment of Obesity in Children and Adolescents
- Caring for the Bariatric Patient
- General Strategies for Overweight and Obesity Prevention and Advocacy
- Conclusion
- Resources
- References
INTRODUCTION
According to the World Health Organization (2022a), obesity has reached epidemic proportions around the globe, nearly tripling since 1975. Today, most of the world’s population lives in countries where being overweight or obese causes more deaths than being malnourished and underweight.
The fundamental cause of overweight and obesity is an energy imbalance that results from consuming more calories and expending less energy. Around the world there has been an increase in the intake of energy-dense foods and a decrease in physical activity due to the increasingly sedentary nature of many types of work, changing modes of transportation, and increasing urbanization.
These are often the result of environmental and societal changes associated with development and the lack of supportive policies in the areas of health, agriculture, transport, urban planning, environment, food processing, distribution, marketing, and education (WHO, 2022a). This global problem has profound social, economic, and health implications for individuals and communities.
Defining Obesity
Obesity is defined by the Obesity Medicine Association (2021) as “a chronic, relapsing, multifactorial, neurobehavioral disease, wherein an increase in body fat promotes adipose tissue dysfunction and abnormal fat mass physical forces, resulting in adverse metabolic, biomechanical, and psychosocial health consequences.”
The American Medical Association (2013) classified obesity as a disease after an overwhelming vote in favor and defined it as a state of excessive fat accumulation that presents a risk to health. Classifying obesity as a disease is the first step toward objectively assessing the factors that lead to it and working toward its prevention and treatment. Some have countered this by saying that obesity is a risk factor for disease but not a disease itself. By such reasoning, however, a condition such as hypertension should not be classified as a disease.
Arguments for why obesity is a disease and not merely an aesthetic issue include:
- Genes may play a role, as well as other diseases or disorders, such as hypothyroidism, Cushing’s disease, and polycystic ovarian syndrome.
- Taking certain medications for other health conditions can lead to weight gain (e.g., antidepressants).
- Each person has their own base metabolic rate, so for two people who are the same height and eat the same diet, one may be obese while the other is not.
- Some aspects of obesity are preventable; however, it is known that some people may make appropriate changes in diet and exercise yet still be unable to lose significant amounts of weight.
Arguments made by those who believe obesity is not a disease include:
- There is no clear way to measure obesity. Body mass index does not apply to everyone (e.g., endurance athletes and weightlifters).
- Obesity doesn’t always reflect poor health. It can be a risk factor but does not always cause negative effects.
- Defining obesity as a disease may foster a culture of personal irresponsibility.
- Defining obesity as a disease may increase discrimination for those with obesity.
Obesity is a complex, multifactorial disease scientifically shown to be brought on and sustained by many factors both within and beyond the individual’s control. Much research has been done and continues to be done into what has now been clearly identified as a major disease state involving personal, societal, and environmental factors. Attitudes must shift from solutions that emphasize an individual-oriented responsibility to include these factors, and healthcare professionals must strive to eliminate stigmatizing individuals with excessive weight and obesity in order to provide the healthcare they require.
HOW OVERWEIGHT AND OBESITY ARE DETERMINED
To determine whether an individual is overweight or obese, a common, inexpensive, albeit imperfect, measure of obesity is the body mass index (BMI), a person’s weight (in kilograms) divided by the square of their height (in meters). A person with a BMI ≥25 kg/m2 is considered overweight, ≥30 obese, and ≥40 severely (morbidly) obese (WHO, 2022a).
For example, a person who weighs 132 kg (291 pounds) and stands 1.83 meters tall (6 feet) has a BMI of 132 divided by 1.832, or 39.4 kg/m2, which is considered obese.
(See also “Body Mass Index” later in this course.)
Scope of the Problem
GLOBALLY
In 2020, there were an estimated 500 million adults in the world who were obese and nearly 1.8 billion adults 18 years and older who were overweight. In 2020, 39 million children under the age of 5 and over 340 million children and adolescents ages 5–19 were overweight or obese. It is estimated that if the issue is not adequately addressed, an estimated 1 billion adults will be obese by 2030.
In 2021, the small island nation of Nauru in the southwestern Pacific had a 61% obesity prevalence, the highest in the world; the country with the lowest prevalence (2%) was Vietnam (CDC, 2021a; WPR, 2021).
IN AMERICA
Obesity affects some groups in the United States more than others:
- By race/ethnicity, non-Hispanic Black adults had the highest age-adjusted prevalence of obesity, followed by Hispanic adults, non-Hispanic White adults, and non-Hispanic Asian adults.
- By age:
- More than 1 in 3 adults and about 1 in 5 children are considered to be obese.
- Obesity prevalence was 40% among adults ages 20–39 years, 45% among adults ages 40–59 years, and 43% among adults ages 60 and older.
- The obesity rate among youth ages 2–19 years is nearly 20%, or about 14.4 million in total.
- By sex:
- Overweight and obesity in adults have increased from 21% in men and 24% in women to almost 40% in both sexes in the past four decades.
- The percentage of men who are defined as overweight is higher than that of women, but the percentage of women who have severe obesity is higher than that of men with severe obesity.
- By educational level, men and women with college degrees had lower obesity prevalence compared with those with less education.
- By income:
- Among non-Hispanic White and Hispanic men, obesity prevalence was lower in the lowest and highest income groups compared with the middle-income group.
- Among non-Hispanic Black men, obesity prevalence was higher in the highest income group compared to the lower.
- Among non-Hispanic White, non-Hispanic Asian, and Hispanic women, obesity prevalence was lower in the highest-income group compared to the middle- and lowest-income groups.
- Among non-Hispanic Black women, there was no difference in obesity prevalence by income.
GEOGRAPHIC DISPARITIES IN OBESITY
Obesity prevalence varies across states and territories. Regionally, the Midwest and South have the highest prevalence of obesity, followed by the West and the Northeast.
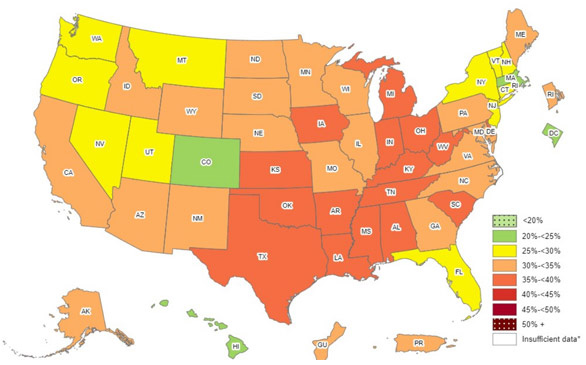
Prevalence of self-reported obesity among U.S. adults by state and territory. (Source: CDC, 2021c.)
ECONOMIC AND SOCIAL IMPACTS
Obesity and the associated health problems that develop as a result have a significant economic impact on the U.S. healthcare system, having risen to nearly $1.4 trillion and equaling 6.76% of the Gross Domestic Product (GDP) in 2018. This includes both direct and indirect costs. Direct costs may be incurred for preventive care services, diagnostic testing, and treatment. Indirect costs related to illness and death are estimated at over $1 trillion for lost workdays or decreased productivity at work.
In 2019 adult obesity was linked to $3,097 in excess annual costs per person, and childhood obesity was associated with over $100 per child. Healthcare expenditures for children with severe obesity have increased by $300 per year.
Obesity-related costs increase with age, starting at around age 30 and increasing until about age 65, at which point the gap between obesity and nonobesity begins to narrow. This is partly due to increasing costs as a result of aging among those with a normal weight and increased mortality among individuals with severe obesity.
Overall per capita spending is higher for adult women than adult men but lower for girls and boys. The highest estimated costs occur in 60- to 70-year-olds.
Medical expenses and lost workdays among obese individuals represent only a portion of obesity-related costs. Other related costs can include the necessity for informal caregivers and lost productivity.
In addition, there are social and emotional effects of obesity, including discrimination, lower wages, lower quality of life, and an increased risk for depression (Milken Institute, 2020; Ward et al., 2021).
OBESITY AND COVID-19
More than 900,000 adult COVID-19 hospitalizations occurred in the United States between the start of the pandemic and November 2020. Models estimate that 271,800 (30.2%) of those hospitalizations were attributed to obesity. Obese children diagnosed with COVID-19 have a 3-times higher risk of hospitalization and 1.5-times higher risk of severe illness when hospitalized.
(CDC, 2021b)