PATHOPHYSIOLOGY OF COPD
In COPD, the body’s reaction to inhaled pollutants (mainly smoke) results in chronic inflammation of the bronchial tree. Inflammation is a natural protective reaction, but it is useless against air pollutants. Instead of helping, the persistent inflammatory reactions damage the lungs.
Normal Lungs
Understanding the structure and function of normal lungs is helpful to understanding COPD’s inflammatory damage.
LUNG STRUCTURE
The two lungs comprise millions of microscopic alveoli clustered at the ends of tiny air tubes. The lung tubes begin at the trachea and branch into successively narrower, shorter, and more numerous tubules. The central tubes are the bronchi and bronchioles. The most peripheral tubes are the respiratory bronchioles, which are lined with alveoli. It is through the walls of the alveoli that gases are exchanged between the inspired air and the blood in the surrounding capillaries.
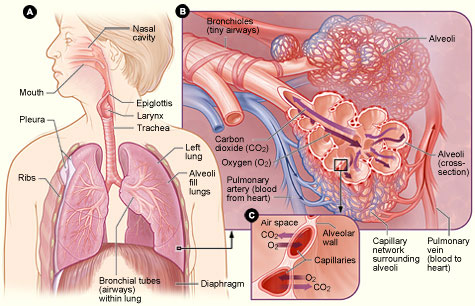
Figure A: Locations of the respiratory structures in the body.
Figure B: Enlarged image of airways, alveoli, and their capillaries.
Figure C: Location of gas exchange between the capillaries and alveoli.
(Source: National Institutes of Health.)
The medium and large bronchi are wrapped with smooth muscle, which tightens to narrow the airways and relaxes to widen the airways. The walls of all the airways are lined by ciliated epithelial cells with interspersed secretory cells, which coat the inner walls of the airways with mucus. All the cilia of the pseudostratified epithelial cells beat in the direction of the trachea and throat, so mucus and trapped particles are continuously moved up and out of the lungs.
Healthy lungs are lightweight, soft, spongy, and elastic. The anatomy of the lungs promotes gas exchange between the circulatory system and the source of oxygen in air. Normally, the chest walls stretch the lungs and keep them expanded to three times their relaxed size. When the chest is surgically opened, however, the lungs recoil, as the innate elasticity of the lungs pulls them back to their resting size (Haddad & Sharma, 2021).
When an adult takes a full breath, the volume of air in the lungs is about six liters on inspiration. During life, the lungs are never completely empty; even after a complete exhalation, there are about 2.5 liters of air left.
LUNG FUNCTION
Lungs are the organs through which oxygen is absorbed into and carbon dioxide is expelled from the bloodstream. These gas exchanges occur through the walls of the alveoli and the terminal respiratory airways, which make up the distal-most air spaces inside the lungs.
Maintaining healthy levels of blood gases are the lungs’ primary function, and the lungs contain an extensive capillary system to provide more than the necessary surface for gas exchange. The lung tissue itself is very thin and delicate, and most of the volume inside a normal lung is taken up by air. Since lung tissue is thin and air is light, most of the weight of a lung can be attributed to the blood circulating in it (Haddad & Sharma, 2021).
People with healthy lungs rarely use all the gas-exchange potential of their lungs. During the most strenuous activity, a healthy person will use only 60% to 70% of their maximal ventilatory capacity. Strenuous exercise does cause temporary dyspnea, but the 30% to 40% ventilatory reserve quickly relieves the dyspnea of a healthy person after a short rest. Even the dyspnea caused by strenuous exercise in a healthy person is not as debilitating as the dyspnea in a person with severe COPD.
Healthy lungs function less efficiently as they age. As people get older, their chest walls stiffen, bones become weaker, and respiratory muscles weaken. These changes make breathing almost twice as much work for a 70-year-old as for a 20-year-old. The forced vital capacity (VC or FVC) and the amount of air that can be exhaled in one second (1-second forced expiratory volume, or FEV1) gradually and progressively decline during a person’s lifetime. In a healthy person, none of these natural lung changes approaches the dramatic declines caused by COPD. The natural decline in lung function worsens the already compromised breathing of those older adults who have COPD (Harding et al., 2020).
Lungs with COPD
COPD slowly destroys the lungs and makes it increasingly difficult for a patient to breathe. The most serious effect of COPD is a progressive obstruction of airflow.
In COPD the airways leading into the alveoli become narrowed and less flexible, and they are often clogged with mucus. Eventually, many alveoli coalesce into larger, useless airspaces because the walls separating the alveoli become damaged or destroyed.
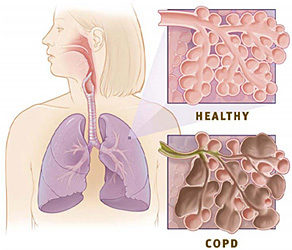
Upper right: Healthy alveoli.
Lower right: Alveoli with COPD.
(Source: National Institutes of Health.)
The specific form that COPD takes varies from person to person. The two predominant forms of COPD are emphysema (destruction of alveoli) and chronic bronchitis (inflammation of the conducting air tubules).
EMPHYSEMA
For some people, COPD causes significant destruction of the terminal airways and air alveoli. This form of COPD is called emphysema. In emphysema, the overall architecture of the lung is altered dramatically and the lung becomes honeycombed with useless spaces. These air spaces are created when the walls of the small respiratory airways and their alveoli are torn, allowing neighboring airways and alveoli to merge.
In the process, the surrounding capillaries become damaged, resulting in reduced pulmonary perfusion. Another characteristic of emphysema is decreased elasticity of lung tissue, resulting in reduced recoil and increased stiffness. Besides reducing the lung area available for gas exchange, emphysema leads to hyperinflated lungs and obstructed airflow (Harding et al., 2020).
CHRONIC BRONCHITIS
The other main type of COPD involves inflamed airways that become clogged with mucus produced by the goblet cells in the lungs. Patients with this variant of COPD develop a chronic cough that brings up sputum. This manifestation of COPD is a form of chronic bronchitis, which is defined as a persistent mucus-filled cough that has occurred frequently for at least three months per year in two consecutive years and that is not caused by another disease such as an infection, cancer, or congestive heart failure. It is characterized by an increase in the number and the size of mucous glands in the airways of the lung.
Chronic bronchitis can occur without COPD. More than one third of smokers have chronic bronchitis, but the disorder is only considered a form of COPD when there is also significant obstruction to airflow within the lungs (Harding et al., 2020).
Contributors to COPD
In the industrialized world, cigarette smoking is the main cause of COPD. In underdeveloped countries, smoke from plant products that are burned for indoor cooking or heating is as much a cause of COPD as is cigarette smoking.
The global prevalence of smoking is 22.7% of the population over age 15. This is approximately 1.3 billion people. There are 8 million deaths annually due to smoking—approximately 7 million as a direct result of smoking cigarettes and 1.2 million a result of second-hand smoke. In the United States the death toll is estimated to be 480,000 every year (WHO, 2021).
In the United States, chronic lung diseases, including COPD, account for 75% of smoking-related conditions. People who have never smoked account for 25% of all COPD cases. Other smoking-related diseases or conditions include throat cancer, stroke, heart attack, and asthma. Other irritants that may cause COPD are air pollution, environmental or workplace chemical fumes or dusts, and second-hand smoke (NIH, 2021a; NIH, 2021b).
Many long-term smokers eventually develop COPD, but the severity of the disease varies from person to person, even among heavy smokers. People living in the same environment and smoking the same amount can differ in their propensity for developing COPD. Two factors have been suggested as the basis for this difference: individual physical characteristics and genetic factors (Harding et al., 2020). The longer and more intensely people smoke, the more likely they are to develop COPD.
People who experience extensive exposure to second-hand smoke (SHS) have a considerably higher occurrence of respiratory symptoms, asthma, and COPD. Of the more than 20,000 participants included in one recent study in Denmark, 12% who had seen lifelong exposure to second-hand smoking, 2% who had been exposed in adulthood only, and 69% who had been exposed in childhood only exhibited the respiratory symptoms of COPD or were diagnosed with COPD or asthma. Similar studies in other countries, although with smaller study samples, show the same compelling results, with a direct correlation between extended exposure to SHS and the eventual development of COPD (Korsbaek et al., 2021).
INFLAMMATORY RESPONSE
Cigarette smoking causes COPD by inciting a chronic inflammatory response to the pollutants in the smoke. This persistent inflammation is caused by the release of proteases in the lungs and eventually leads to destruction of lung tissue, accumulation of mucus, and thickening of small airways. Smoke also flattens the cilia in the airways and prevents them from removing mucus and fluid. Prolonged pulmonary inflammation is eventually accompanied by systemic inflammation.
Other factors such as inhaled pollutants, sedentary lifestyle, and infections may also contribute to systemic inflammation in someone with COPD. The severity of inflammation may necessitate the use of corticosteroids. Patients with COPD are more resistant to the effects of corticosteroids, requiring higher doses and more prolonged use than more healthy smokers or nonsmokers. When treatment of COPD with steroids requires prolonged usage or higher dosages, COPD patients are more susceptible to developing pneumonia. Some COPD patients are resistant to steroids, requiring either a higher dosage or becoming unable to take steroids effectively (Beaumont, 2018).
Destruction of Lung Tissue
Lungs with COPD produce less enzymes that promote the formation of myofibroblast cells to aid in the healing of wounds and tissue. In the absence of this enzyme (alpha–smooth muscle actin, or α-SMA), diseased lung tissue in COPD is repaired more slowly (Holm Nielsen et al., 2019). The progressive destruction of lung tissue leads to the emphysematous form of COPD, which is characterized by:
- Destruction of alveoli
- Loss of lung elasticity
- Loss of lung supporting tissue
- The collapse of small airways
(Harding et al., 2020)
Thickening of Small Airways
The hallmark of COPD is the increased resistance it causes for airflow in the lungs. In the chronic bronchitis form of COPD, much of the airflow obstruction comes from a progressive thickening and stiffening of the small airways in addition to increased mucus production. The pathologic process underlying the narrowing of airways is fibrosis. With fibrosis, excess collagen accumulates in and around the airways, making them fatter and more rigid. Extra collagen is secreted as a natural repair response to tissue damage. In COPD, myofibroblasts produce lower-than-normal levels of α-SMA, inhibiting the natural repair response (Holm Nielsen et al., 2019).
The chronic bronchitis form of COPD includes changes in the small airways. These changes reduce airway volume. Specifically:
- Mucous cells proliferate and become larger; this generates excess mucus.
- The smooth muscle in the airway walls thickens.
- The airway walls bulge with invading inflammatory cells.
AIRWAY SENSITIVITY
People differ in their airway sensitivities, that is, in how readily their airways constrict when exposed to a variety of irritants such as pollen, dust, and chemicals. Asthma is the most common disease of people who have abnormally sensitive airways. People with COPD also tend to have sensitive and reactive airways. Although asthma and COPD are different diseases, smokers with asthma or with the tendency to develop asthma are more likely to develop COPD and are more likely to have COPD that worsens quickly (Harding et al., 2020).
ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
Besides airway sensitivity, certain genetic factors make some individuals especially susceptible to developing COPD. One of these genetic propensities is an autosomal recessive disorder called alpha-1 antitrypsin deficiency. The gene for AAT is recessive. Therefore, someone with one normal and one faulty allele for the deficiency would be a carrier but not more susceptible to COPD. People of northern European descent are affected the most.
AAT deficiency allows the chronic inflammation caused by inhaled smoke to do considerable damage to the lungs; specifically, AAT deficiency fosters the destruction that causes emphysema. AAT is produced by the liver, and a deficiency can produce liver as well as lung disease.
Long-time smokers typically develop COPD when they are 50 to 60 years old, but smokers who are born with AAT deficiency develop symptomatic COPD 10 to 20 years earlier, at an average age of 40 years. Elastase is so destructive that emphysema can even develop in nonsmokers if they have a severe AAT deficiency (GOLD, 2021; Harding et al., 2020).
Treatment is the replacement of the deficient AAT with the drug Prolastin (alpha).
ELECTRONIC CIGARETTES AND COPD
Electronic cigarettes (e-cigarettes) were invented in 2004. They may also be referred to as e-cigs, e-hookahs, mods, vape pens, vapes, tank systems, and nicotine delivery systems (ENDS). These devices evaporate a liquid made of humectants (propylene glycol and glycerol), flavorings, and nicotine. An e-cigarette system consists of a cartridge filled with the e-liquid, a heating element or atomizer to heat the e-liquid and create a vapor that is inhaled through a mouthpiece, and a rechargeable battery to operate the system (Marques et al., 2021). Smoking an e-cigarette is commonly referred to as vaping (CDC, 2021d).
Vaping can help facilitate tobacco smokers to reduce or quit smoking altogether. In 2018, a randomized trial in the United Kingdom compared the use of e-cigarettes and nicotine replacement (patch, gum, lozenge, nasal spray, inhalator, mouth spray, mouth strip, and microtabs) as smoking cessation interventions. The success rate for quitting smoking was found to be twice as high in the e-cigarette group (18%) than in the nicotine-replacement group (9.9%) after one year (Marques et al., 2021).
Other studies have weighed the relative risks and benefits of the use of e-cigarettes vs. conventional cigarettes. Tobacco smokers who substitute e-cigarettes for conventional cigarettes are exposed to less toxins and may experience a longer life expectancy. The possible negative effects of e-cigarettes depend on the components contained within the device. A recent study of e-cigarette or vaping product use–associated lung injury (EVALI) showed an increase in inflammation in the lungs and impaired gas exchange caused by the aerosolized oils within the e-cigarettes. Most of the e-cigarettes that cause these types of injuries involve tetrahydrocannabinol (THC) as the active ingredient (Marques et al., 2021).
However, there is also compelling evidence that people who had not previously smoked conventional cigarettes, especially adolescents and young adults, may progress from vaping to cigarette smoking and subsequently become addicted. E-cigarettes contain nicotine, often in remarkably high amounts. In adolescence, nicotine can harm the parts of the brain that control attention, learning, mood, and impulse control. Adolescent brains build synapses faster than adult brains, and nicotine changes the way these synapses are formed. For that reason, smoking e-cigarettes is considered to produce more risks than benefits (CDC, 2021d).
The effects of vaping by persons with COPD include additional inflammation of lung tissue, most noticeably in the bronchial epithelial cells. The chemicals in e-cigarettes cause a toxic response in the lung tissue and reduce the ability of the lungs to respond defensively to viral infections. Many of the flavors contained in the aerosolized liquid in e-cigarettes produce substances that have deleterious effects on human embryonic stem cells and human pulmonary fibroblasts. A partial list of these chemical substances include cinnamaldehyde, diacetyl, 2,3-pentanedione, acetoin, and benzoic acid. Of note, the flavors bubblegum, butterscotch, and caramel produce no cytotoxicity (Marques et al., 2021).
Multiple studies have been conducted regarding the effects on persons with COPD who smoke marijuana through the use of e-cigarettes. It was thought that there might be some benefit with additional bronchodilation for those with COPD from vaping marijuana. It is considered less harmful to the lungs than more traditional methods of smoking the drug but can still cause an injury. In fact, THC products have been found to play a role in lung injury caused by the use of e-cigarettes (CDC, 2019).
ANSWERING PATIENT QUESTIONS
Q:What causes COPD?
A:Smoking is the most common cause of COPD. Cigarette, cigar, and pipe tobacco can all cause COPD when the smoke is inhaled. Other kinds of air pollution can be just as bad as smoke if the pollution is inhaled for many years.
Anyone can get COPD from smoking, although it usually takes many years of smoking for the disease to be noticeable. A small number of people also have an inherited genetic defect called AAT deficiency.
Q:Can COPD be inherited?
A:Most types of COPD are not inherited. COPD is usually caused by cigarette smoking. Teaching children not to smoke will help protect them from getting COPD. A small number of people inherit a genetic defect called AAT deficiency, which makes them more likely to get the disease after only a few years of smoking or sometimes without having ever smoked at all. When these people get COPD, it is the emphysema type of COPD, and it usually shows up early, in people younger than 40 years old.
Q:Is COPD contagious?
A:No.
Functional Effects of COPD
REDUCED FEV1
When inhaling, a person stretches their chest and lung tissues. During exhalation, the elastic recoil of the chest and lungs is a major contributor to the force that pushes air out of the lungs. Failure to force a sufficient amount of air out of the lungs upon expiration causes the buildup of carbon dioxide (CO2) in the lungs and then in the blood (hypercapnia).
In COPD, fibrosis reduces lung elasticity. Therefore, a patient with COPD needs to replace the lost elastic force with extra muscular effort, and the extra effort must be sustained for a longer time. The narrowed airways in lungs with COPD carry smaller volumes of air, and people with COPD take longer to empty their lungs.
The extent of airway obstruction can be quantified for patients with COPD. One standard assessment measures the patient’s 1-second forced expiratory volume (FEV1), the volume of air that can be pushed out of the lungs during the first second after a full inhalation after the patient has taken a bronchodilator. A persistent, irreversible low FEV1 (≤70%) is the most characteristic objective finding in COPD (GOLD, 2021; Harding et al., 2020). (See “Lung Function Tests” below.)
HYPERINFLATION OF THE LUNGS
In COPD, the difficulty of breathing is worsened by excessively expanded (hyperinflated) lungs. Most people with COPD have some degree of emphysema, and part of each breath flows into nonfunctioning spaces, where it is unusable. To get sufficient oxygen into their system, people with COPD need to take larger breaths.
People with COPD also take longer exhaling, and after taking a large breath, in spite of the use of accessory muscles of respiration, there is not enough time to fully exhale the air. Excess air remains in their lungs during each breathing cycle.
Wasted air space and excess residual air lead to hyperinflated lungs. Hyperinflated lungs change the shape of the chest and diaphragm (described as barrel chest), making the mechanics of breathing more difficult. With hyperinflated lungs, breathing can be exhausting.
HYPOXEMIA AND HYPERCAPNIA
Together, the obstructed airflow and the hyperinflated lungs of COPD make breathing arduous work. When COPD is severe, just the breathing required for slow walking could use one third of the body’s total oxygen intake.
In COPD, patients may not have enough energy to pull in all the oxygen they need or to expel all the carbon dioxide they produce. Compounding the problem of maintaining adequate gas exchange, COPD destroys alveoli and the small capillaries that surround them, making each breath even less effective.
As a result, people with severe COPD become chronically hypoxemic (too little circulating oxygen in the blood) and hypercapnic (too much circulating carbon dioxide in the blood). People with moderate COPD become hypoxemic during modest exercise, and as the disease worsens, they can become unable to exercise at all.
DYSPNEA AND ITS SPIRALING EFFECTS
Over the years, patients with COPD become less and less able to do even modest exercise without developing dyspnea. Dyspnea is the most frequently reported symptom in patients with moderate and severe COPD. The degree of dyspnea is self-reported by the patient, similar to pain levels. The symptom burden for patients with COPD can be compared to the symptom burden of lung cancer patients. It comes from a mix of three sensations:
- The urge to breathe. This sensation is triggered by exercise or by the metabolic results of exercise: hypoxemia, hypercapnia, and metabolic acidosis.
- Difficulty breathing. This sensation is produced by excess chest movement and by unusual effort required by the muscles of respiration during breathing.
- Anxiety. This sensation can be caused by a fear of suffocating or by a memory of past discomfort with breathlessness. The anxiety of dyspnea can also come from entirely dissimilar sources of stress that are happening at the time, such as emotional and psychosocial factors like anxiety or depression.
(Basara et al., 2018)
Breathlessness is upsetting. It stops people from exercising, and it is the main reason that people with COPD limit their activities. Dyspnea with exercise gets worse as COPD progresses. The degree of perceived breathlessness is proportional to respiratory effort. Exertional dyspnea may be caused by hyperinflation of the lungs from trapped air, resulting in reduced inspiratory volume. Patients begin to spend all their time either sitting in a chair or lying in bed, and after months of inactivity, patients with COPD become deconditioned as their muscles and circulatory system settle into sedentary states.
The pain and dyspnea that accompany COPD make it even more difficult to exercise. It is a spiraling problem: dyspnea causes lack of exercise, lack of exercise causes deconditioning, and deconditioning makes it harder to exercise. When they have become deconditioned, patients with COPD get severe leg tiredness and leg pain when they try to exercise. Leg problems become yet another limiting factor when deconditioned people with COPD attempt to exercise (Moy et al., 2021).
To break this cycle, people with COPD must exercise. Pulmonary rehabilitation—which includes gradually increasing, supervised training regimens—can reverse muscle weakness, reduce leg pain, and increase exercise tolerance (ALA, 2021). (See “Pulmonary Rehabilitation” later in this course.)
Damage Beyond the Lungs
Patients with COPD have problems with organ systems other than their lungs. COPD leads to chronic hypoxemia, drains energy reserves, and is a source of chronic inflammation. These problems cause total-body muscle weakness and weight loss.
Chronic hypoxemia strains the heart and reduces the ability of the heart’s ventricles to respond to the demands of exercise. This may lead to ischemic tissue and heart failure. Caution must be taken in the pulmonary rehabilitation phase of treatment to prevent symptomatic ischemia.
Chronic inflammation initiates a generalized prothrombotic condition in the circulation. This makes blood clots more likely to form, and patients with COPD are at increased risk for developing myocardial infarctions (MIs), cerebral vascular accidents (CVAs), deep vein thromboses (DVTs), and pulmonary emboli (PEs).
CASE
Marilyn, a 72-year-old woman, presents to the emergency department with shortness of breath; tachypnea; and pain, heat, and redness in her right calf. She has a 40 pack-year history of smoking and quit 10 years ago when she was diagnosed with COPD. Contrast venography is performed to the right leg, and the radiologist diagnoses deep vein thrombosis. During the history taking, the patient states she just returned from a trip to visit her grandchildren, who recently moved across the country, and that the leg pain started soon after the long airplane flight.
The emergency department nurse explains to Marilyn and her family that patients with COPD are at higher risk for DVT due to the chronic inflammation in the blood vessels caused by cigarette smoking. Once the COPD process starts, quitting smoking does not improve the problem.
Marilyn will be admitted to the hospital and started on anticoagulant therapy to prevent more clots from forming and an exercise regime initiated by physical therapy.
PULMONARY HYPERTENSION IN COPD
Changes caused by COPD increase the arterial resistance inside the lungs. These include:
- Destruction of lung capillaries
- Thickened walls of small pulmonary blood vessels
- Constricted lung arteries due to chronic hypoxia and acidemia (a blood pH of <7.35 caused by greater-than-normal concentration of hydrogen ions)
- Constricted lung arteries due to the physical pressure of hyperinflated lungs
Due to these changes, more force is needed to push blood through the lungs, and the person develops pulmonary hypertension. Pulmonary arterial hypertension (PAH) is chronic, progressive, and results in an increased pulmonary arterial pressure because of the constriction on the pulmonary blood vessels caused by alveolar hypoxia. In a normal adult lung, the mean pulmonary artery pressure is 12–16 mmHg. In a lung with pulmonary hypertension, the mean pulmonary artery pressure is >25 mmHg at rest and >30 mmHg with exercise.
Pulmonary hypertension is especially hard on the right ventricle of the heart, which hypertrophies in response. Pulmonary hypertension can exist comorbidly with other diseases such as heart failure and COPD. As the strain on the right ventricle persists, the heart can fail. Heart failure secondary to lung problems is called cor pulmonale, and COPD is the leading cause of cor pulmonale as a late manifestation of the lung disease. The incidence of pulmonary hypertension in COPD is around 20% but more than 50% in severe chronic bronchitis (Harding et al., 2020).
DEPRESSION
People with COPD have a high incidence of clinical depression (16.2%) and anxiety (15.9%). The presence of these two psychological clinical characteristics increases mortality in COPD patients by 21%. The depression is not only a psychological reaction to their increasingly restricted lifestyles. There is a demonstrated increase in patients with COPD with depression when there is evidence of clinical determinants such as poorer health, living alone, female gender, diabetes, and lower income (Vikjord et al., 2020).