RISK FACTORS FOR ABUSIVE HEAD TRAUMA
Anatomy- and Physiology-Related Risk Factors
There are specifics risks to the young infant due to their anatomy and physiology. These include the combination of a disproportionally larger head, soft and rapidly growing brain, thin skull wall, and lack of mobility and control of the head and neck that makes infants extremely vulnerable to injury from shaking actions.
Because the brain grows rapidly during infancy, infants have proportionally larger heads than adults in relation to their body size. (The relation between head and body size continuously declines with increasing age.) Therefore, the head is relatively heavy compared to the rest of the body, which results in different dynamics of head acceleration due to external forces, making the infant head more vulnerable to trauma (Araki et al., 2017).
Additionally, the infant’s brain has higher water content and less myelination than an adult brain, is more gelatinous, and is easily compressed and distorted within the skull during a shaking episode. The infant’s blood vessels around the brain are more susceptible to shearing, and tearing can lead to brain hemorrhages. Because of their minimally developed anatomy, infants are also at increased risk for death and permanent disability.
It is also important to take into account that the immature brain requires a different balance of neuro transmission, blood flow, and energy requirements that may predispose it to a poorer injury phenotype. Trauma during this period may also interfere with ongoing developmental events such as neuronal migration and axonal and dendritic growth by altering the proteins that guide these processes (O’Meara et al., 2020).
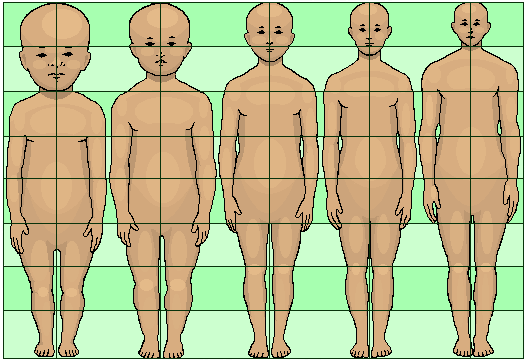
Diagram showing the proportionally larger head of an infant relative to an adult. (Source: Journal of Heredity, 1921.)
Household Risk Factors and Perpetrator Characteristics
Understanding the AHT risks from various caregivers may help to inform current prevention strategies. A critical risk factor is the occurrence of shaking used either to attempt to calm infants and children or as a means of discipline. Less consistent risk factors include socioeconomic status, societal and family stress, prematurity, multiple births, developmental delay, prior military service, and childhood history of abuse in the perpetrator (Joyce & Huecker, 2018).
There are few statistics looking specifically at risk as it relates to perpetrators of pediatric AHT. Among the limited studies, Ahmed (2017) reported that “by far, parents were more likely to be perpetrators of the confirmed or suspected child abuse. However, children injured by a parent’s partner—a group that was overwhelmingly male—were more likely to be more severely injured, to experience severe head injuries, and to require intubation compared with children who were abused by a parent.” Laurent-Vannier and colleagues (2021) examined 91 cases of AHT and found that all of the abusive events occurred inside a home (parent’s or childcare provider’s), never outdoors or in a public place, and always in the presence of only one adult. One third of perpetrators were males (n=32), and two thirds females (n=59), of which 49 were the childcare provider (“nanny”) and 10 were the infant’s mother.
According to the CDC (2022), factors that increase the caregiver’s risk for child abuse in general include:
Individual Risk Factors
- Parents’ lack of understanding of children’s needs, child development, and parenting skills
- Parental history of child abuse and/or neglect
- Substance abuse and/or mental health issues, including depression in the family
- Parental characteristics such as young age, low education, single parenthood, large number of dependent children, and low income
- Nonbiological, transient caregivers in the home (e.g., mother’s male partner)
- Parental thoughts and emotions that tend to support or justify maltreatment behaviors
Family Risk Factors
- Social isolation
- Family disorganization, dissolution, and violence, including intimate partner violence
- Parenting stress, poor parent-child relationships, and negative interactions
Community Risk Factors
- Community violence
- Concentrated neighborhood disadvantage (e.g., high poverty, residential instability, high unemployment rates, and high density of alcohol outlets) and poor social connections
Child Risk Factors
Children with special needs—including those born prematurely and/or having developmental delays and/or disabilities—are at higher risk for AHT. A lack of understanding of premature infant development may lead to additional frustration, stress, decreased tolerance, and resentment among caregivers. Since premature infants have a higher rate of disabilities than full-term infants, their risk is even greater.
Infants experiencing neonatal abstinence syndrome (NAS) (i.e., babies in withdrawal) are at particular risk for child abuse, including abusive head trauma, due to the irritability and excessive crying that result from withdrawal from substance addiction. This can last for weeks and months, making such babies difficult to care for.
Additionally, the CDC (2022) reports that the following characteristics also increase an infant’s risk for being shaken, particularly when combined with a parent or caregiver who is not prepared to cope with caring for a baby:
- A history of previous child abuse
- Infant prematurity or disability
- Being one of a multiple birth
- Being less than 6 months of age
- Being perceived as inconsolable and/or crying frequently
CASE
Jasper is 3-1/2 months old and was born prematurely at a gestational age of 34 weeks. He was admitted to the ED after his father called 911 because Jasper turned blue while being bottle-fed. Emergency personnel had started CPR because Jasper was not breathing and they were unable to get a pulse. Jasper had been seen by his primary care physician three times since his discharge from the neonatal intensive care unit and has been diagnosed with colic, feeding difficulties, and possible gastro-esophageal reflux.
Jasper was initially resuscitated in the ED, and once he was stable, an evaluation revealed multiple injuries consistent with pediatric AHT. Jasper was transferred to a regional pediatric intensive care unit and was removed from life support three days later because he had irreversible brain stem dysfunction.
Jasper’s father later reported that Jasper’s mother had just returned to work after six weeks of parental leave. He had agreed to look after the infant, but he lost his temper and shook Jasper because he kept on crying and refusing the bottle.