BIOLOGICAL TERRORISM PREPAREDNESS AND RESPONSE
Biological terrorism involves the use of a microorganism (or a toxin derived from it) that causes disease in persons, plants, or animals or causes the deterioration of material (DOD, 2021). These pathogens may be bacteria, fungi, toxins, parasites, protozoans, or viruses. They can be naturally occurring, and/or they may be altered in a laboratory to increase their resistance to antibiotics or their ability to spread in the environment.
Biological weapons are a common choice for terrorist organizations due to their ease of being deployed, the devastating effects they cause, and how inexpensive they are to produce. There is, however, an unpredictability in that these weapons may affect the intended victims and, inadvertently, the perpetrators (Rathish et al., 2021).
Mode of Transmission
Biological agents can be very difficult to detect, and many do not cause illness for several hours or even days. These agents are most likely to be dispersed as aerosols so as to spread among large populations more easily. Some, however, are spread from person to person or by vectors, ingestion, direct contact, or other methods. Water systems are rarely a target; however, water systems have received threats, and because the possibility exists that these threats could be carried out, they must be taken seriously.
While the standard chain of infection applies to diseases caused by exposure to a pathogen, the obvious difference is the mode of transmission link when it is used as a weapon.
- Naturally occurring disease is almost always spread unintentionally. In many cases, it occurs as part of carrying out normal daily activities, with a contaminated hand or uncovered sneeze passing on the infectious agent.
- Intentional spread indicates biological terrorism.
(Rathish et al., 2021; Hayoun & King, 2021)
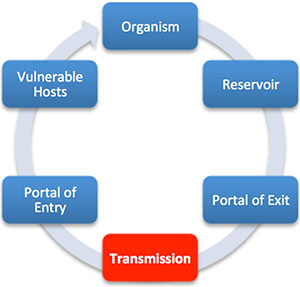
Chain of infection. In biological terrorism, the mode of transmission is intentional. (Source: Wild Iris Medical Education, Inc.)
Bioweapon Classification Categories
The CDC has separated bioterrorism agents into three categories, depending on how easily they can be spread and the severity of illness or death they cause. Factors that contribute to these categories include:
- Ability to have a profound impact on health
- Ability to cause health fears
- Potential for spread
- Availability of protective vaccines or antimicrobial agents
- Secondary transmission potential
- Public health preparedness
CATEGORY A
These high-priority agents include organisms that pose the highest risk to the public and national security because they:
- Can be easily disseminated or transmitted from person to person
- Result in high mortality rates and have the potential for a major public health impact
- Might cause public panic and social disruption
- Require special action for public health preparedness
Category A agents and diseases include:
- Anthrax (Bacillus anthracis)
- Botulism (Clostridium botulinum toxin)
- Plague (Yersinia pestis)
- Smallpox (variola major)
- Tularemia (Francisella tularensis)
- Viral hemorrhagic fevers, including filoviruses (Ebola, Marburg) and arenaviruses (Lassa, Machupo)
(CDC, 2020a)
CATEGORY B
Second highest priority agents include those that:
- Are moderately easy to disseminate
- Result in moderate morbidity rates and low mortality rates
- Require specific enhancements of CDC’s diagnostic capacity and enhanced disease surveillance
Category B agents/diseases include:
- Brucellosis (Brucella species)
- Epsilon toxin of Clostridium perfringens
- Food safety threats (Salmonella species, Escherichia coli O157:H7, Shigella)
- Glanders (Burkholderia mallei)
- Melioidosis (Burkholderia pseudomallei)
- Psittacosis (Chlamydia psittaci)
- Q fever (Coxiella burnetii)
- Ricin toxin from Ricinus communis (castor beans)
- Abrin toxin from jequirity (rosary) peas
- Staphylococcal enterotoxin B
- Typhus fever (Rickettsia prowazekii)
- Viral encephalitis (alphaviruses, such as eastern equine encephalitis, Venezuelan equine encephalitis, and western equine encephalitis)
- Water safety threats (Vibrio cholerae, Cryptosporidium parvum)
(CDC, 2020a)
CATEGORY C
Third highest priority agents include emerging pathogens that could be engineered for mass dissemination in the future because of:
- Availability
- Ease of production and dissemination
- Potential for high morbidity and mortality rates and major health impact
Category C agents/diseases include:
- Emerging infectious diseases such as Nipah virus and hantavirus
(CDC, 2020a)
COVID-19 AND BIOTERRORISM
The intelligence community has begun examining the potential for terrorists to weaponize the COVID virus, particularly against high-level targets. It has been found that the COVID-19 virus, despite the high number of deaths and significant illnesses it has caused, does not have the desired characteristics of a biological weapon. While strains of COVID could be acquired and cultured in a laboratory, its ability to be disseminated from a point or line source is questionable and is too unpredictable as to its effects on a targeted population.
Nevertheless, the COVID pandemic has revealed several weaknesses in government and population response that increase our vulnerability to bioterrorism and reduce our bioweapon deterrence. In addition, adversaries have witnessed this response and can make use of it (Mauroni, 2021).
Category A Diseases with Potential for Use as Bioweapons
ANTHRAX
Bacillus anthracis is a spore-forming organism, with the spores being the infectious element. In its natural state, it is present in the soil, where it may be ingested by grazing animals. It can be transmitted to humans by handling or ingesting contaminated animals, animal products, or soil. Unless exposure is due to an intentional release, anthrax infections are very rare. There are two types of anthrax: inhalation and cutaneous.
ANTHRAX ATTACKS
Seven days after the attacks of 9/11, anonymous letters laced with anthrax began arriving at news media companies and congressional offices. Over the following months, five people died from inhaling anthrax, and 17 others were infected after exposure. Some 10,000 U.S. residents took two months of antibiotics for possible anthrax exposure. Because the anthrax was of weapons grade or near–weapons grade, it appears to have come from a sophisticated laboratory. The perpetrator(s) of these attacks has not yet been identified. Extensive FBI investigations have failed to determine the sender’s exact motive, but the letters included the lines “Death to America,” “Death to Israel,” and “Allah is great” (FBI, n.d.).
Inhalation Anthrax
Inhalation anthrax is considered to be the deadliest form of the disease. Infection usually develops within a week following exposure but can take up to two months. Without treatment, inhalation anthrax is almost always fatal. However, if treated aggressively, about 55% of individuals survive. Inhalation anthrax is not contagious.
| (Mayo Clinic, 2020a; OSHA, n.d.-a, Williams et al., 2021) | |
| Signs/Symptoms |
Initially:
Later:
|
|---|---|
| Treatment |
|
| Personal Protective Equipment |
|
Cutaneous Anthrax
Cutaneous anthrax is the most common form of anthrax infection and is also considered to be the least dangerous. Infection usually begins 1 to 7 days following exposure. This can happen when anthrax spores enter the skin, usually through a cut or scrape, or while handling infected animals or contaminated animal products. Cutaneous anthrax is most common on the head, neck, forearms, and hands. Without treatment, up to 20% of people with cutaneous anthrax die. With proper treatment, almost all patients with this form of anthrax survive.
| (Mayo Clinic, 2020a; Williams et al., 2021) | |
| Signs/Symptoms |
Within 2 weeks of exposure:
|
|---|---|
| Treatment |
|
| Personal Protective Equipment |
|
BOTULISM
Clostridium botulinum is also a soil-inhabiting, spore-forming organism. The neurotoxin it forms is extremely potent and is one of the deadliest toxins known; less than 1 microgram is fatal for adults. It causes difficulty breathing, muscle paralysis, and if untreated, possible death. Botulism can be contracted by ingesting contaminated canned, smoked, or vacuum-packed foods and also by inhaling spores. Human botulism may refer to inhalation, infant, foodborne, or wound botulism. Inhalation of the toxin is rare.
| (CDC, 2021b) | |
| Signs/Symptoms in Adults |
No matter how a person acquires botulism, the symptoms are usually the same, with the defining feature of weakness beginning on both sides of the face, going down the neck and to the rest of the body. Initially:
Other symptoms that can follow:
|
|---|---|
| Signs/Symptoms in Infants |
|
| Treatment |
|
| Personal protective Equipment |
|
PLAGUE
Yersinia pestis is a bacterium that causes acute, potentially fatal infections in both humans and animals. It is naturally occurring in environments in which rats and their fleas exist. Plague has occurred in rural and semi-rural areas of the western United States, primarily in semi-arid upland forests and grasslands. In addition, wild carnivores can become infected by consuming infected prey. Plague can be deadly if not treated promptly with antibiotics. The rarest and deadliest form of plague affects the lungs and can spread from person to person.
Plague is rarely naturally transmitted by inhalation, but that is the most likely means if the organism were to be released intentionally. If released as an aerosol, an outbreak of pneumonic plague is the anticipated result. A plague vaccine is no longer available in the United States. New vaccines are in development but are not expected to be commercially available in the immediate future.
Plague can take different clinical forms, but the most common are bubonic, pneumonic, and septicemic.
Bubonic Plague
Bubonic plague is an infection of the lymphatic system and is usually the result of an infected flea bite. The bacteria multiply in a lymph node near where the bacteria entered and can spread to other areas of the body. Without treatment, the mortality rate is 60%.
| (Minnaganti, 2021; CDC, 2021c) | |
| Signs/Symptoms |
In the first several days:
2–6 days following exposure:
|
|---|---|
| Treatment |
|
| Personal Protective Equipment |
|
Pneumonic Plague
Pneumonic plague may develop from inhaling infectious droplets or from untreated bubonic or septicemic plague that spreads to the lungs. Pneumonic plague is the most serious form of the disease and is the only form of plague that can spread from person to person. Without treatment the mortality rate is 100%, and with treatment it is 50%.
| (Minnagranti, 2021; CDC, 2021c) | |
| Signs/Symptoms |
1–3 days after inhalation:
|
|---|---|
| Treatment |
|
| Personal Protective Equipment |
|
Septicemic Plague
Septicemic plague can occur as the first symptoms of plague or may develop from untreated bubonic plague. This form results from bites of infected fleas or from handling an infected animal. Septicemic plague is frequently associated with delayed diagnosis, and has a higher fatality rate than primary bubonic plague.
| (CDC, 2021c) | |
| Signs/Symptoms |
Acute onset of:
May progress to include:
|
|---|---|
| Treatment |
|
| Personal Protective Equipment |
|
SMALLPOX
The variola virus causes smallpox in two forms. Variola major is the most common and most severe. It has an historical fatality rate of approximately 30%. Variola minor is less common and less severe, with an historical fatality rate of ≤1%.
Smallpox eradication, one of the greatest successes of modern public health, was officially declared worldwide in 1980. The last known case of naturally occurring smallpox was reported in 1977 in Somalia. The last known case in the United States occurred in 1949. Today the smallpox virus is known to exist only in secured research laboratory stockpiles in the United States and Russia. However, advances in synthetic biology have made it possible to create smallpox. Therefore, there is concern that it could someday be used as a biological warfare agent.
Smallpox can be transmitted directly and indirectly from person to person and via contaminated items. Transmission begins with virus particles being sloughed from the oropharyngeal lesions of an infected person. Inhalation of airborne droplets of this saliva introduces the disease to a new host.
The most important way to prevent transmission of smallpox is by vaccination (Harvard Health, 2021).
| (Mayo Clinic, 2020b; Harvard Health, 2021) | |
| Signs/Symptoms |
|
|---|---|
| Treatment |
|
| Personal Protective Equipment |
|
Category B Diseases with Potential for Use as Bioweapons
Ricin and abrin are both biological toxins derived from plants; they are classified as either a biological or chemical weapon. Ricin comes from the beans of the castor plant and abrin comes from jequirity (rosary) peas. One molecule of either toxin is capable of poisoning all of the ribosomes in a cell, leading to cell death. Abrin is more lethal than ricin.
Ricin has been used in injectable form in assassination attempts, but mass casualties would probably involve inhalation of aerosolized toxin.
| (Madsen, 2021; Stoppler, 2020) | |
| Signs/Symptoms |
Inhalational exposure: Latent period of 4–8 hours, followed by:
Ingestion exposure:
|
|---|---|
| Treatment |
First responder:
First receiver:
|
| Personal Protective Equipment |
|
CASE
The largest bioterrorism attack in U.S. history was masterminded by the nurse Ma Puja. In September 1984, five weeks before an election, Ma Puja and eleven other members of the Rajneesh religious cult wanted to affect voter turnout in favor of their candidate for public office. When considering a plan, she reasoned that if the cult could not inflate their own voter numbers, they could suppress everyone else’s by infecting the local water supply with bacteria and forcing large groups of voters to stay at home on election day.
Ma Puja considered a number of different diseases, including typhoid fever, before settling on Salmonella typhimurium, a common cause of food poisoning. This was perfect for her purposes, as it causes severe vomiting and diarrhea but is very rarely fatal. Through her workplace, Ma Puja ordered cultures of Salmonella and the supplies for cultivating them from a medical supply company.
Five weeks before the election, Ma Puja and the eleven others carried out a full-scale dress rehearsal. They targeted the salad and salsa bars of 10 local restaurants and poured Salmonella liquid from concealed plastic bags onto the lettuce, salad dressing, salsa, coffee creamer, and other communal food or condiments at the restaurants.
The rehearsal had dramatic results. More than 150 people fell violently ill with bloody diarrhea, nausea, vomiting, chills, and abdominal pain. Lab tests confirmed infection with Salmonella. By the end of the month, a total of 751 people developed confirmed cases of salmonellosis, and 43 people required hospitalization. None, miraculously, died in the attack.
The attack attracted the attention of the Oregon Public Health authorities, and the increased scrutiny meant the cult members were unable to launch a follow-up attack when election day finally rolled around. Local voters, angered by the cult’s antics, showed up in record numbers to the polls and defeated the cult’s candidate (Manning, 2019; Messier, 2021).