PREVENTIVE FOOT CARE FOR PATIENTS WITH DIABETES
More and more emphasis is now being put on preventive measures rather than exclusively on treatment of diabetes and its complications. Preventing diabetic foot ulcers is of prime importance and must be the focus of every clinician at every encounter with the patient. Prevention of diabetic foot ulcers focuses on two specific factors: foot care and control of the underlying diabetes.
Health and Family History
The first step in preventive care is getting to know as much as possible about the patient’s health history, including family history. Taking time to get to know the patient is critical to successful treatment outcomes. Not only does the clinician glean useful information, most importantly they lay the basis for good rapport with the patient. Questions that the clinician asks are:
- How long since the patient was first diagnosed with diabetes?
- What was the patient’s initial reaction to the diagnosis? Many patients will state that they got “very serious” about their healthcare immediately, while others will describe minimizing the diagnosis, stating that they were “feeling fine” at the time and did not see any need to make changes in their routine or lifestyle.
- What comorbidities does the patient have, such as heart disease, respiratory conditions, or musculoskeletal impairments (UM Health, 2018).
- What is the patient’s level of cognitive function and the presence of depression? A British study reported that up to 40% of individuals with diabetes were affected by depression (Diabetes.co.uk, 2019). A report from the CDC (2021) indicates that persons with diabetes are 2 to 3 times more likely to have depression than persons without diabetes. However, only 25%–50% of those with diabetes and depression receive a diagnosis and treatment.
- Does the patient have a family history of diabetes? If so, how did the family member(s) deal with diabetes and what complications did they have? These are details that can greatly influence how a patient views their own condition. If, for example, a patient’s mother had diabetes and died from heart disease in her mid-50s, the patient may see diabetes as a fatal condition that will greatly shorten their own life.
Limb Assessment
Being aware of the condition of the patient’s lower extremities helps the clinician to identify the patient’s level of risk for developing diabetic foot ulcers, and this will help guide the interventions needed at this stage to prevent ulcers from occurring.
The patient is asked or assisted to remove their shoes and socks, and a careful assessment is made of each leg and foot. Each limb should be compared with the other and any differences between the two of them noted. While assessing the general appearance of the limb, the clinician is observing for the following:
- Color. Paleness may indicate poor circulation, while redness could be a sign of inflammation or the early stages of Charcot osteoarthropathy (degeneration and destruction of weight-bearing joints).
- Dryness. Skin surfaces that are dry, flaking, or cracked may be an indication of impaired circulation.
- Hair distribution on each leg. A lack of hair growth can also be an indication of poor circulation, in particular, arterial circulation.
- Edema. This is determined by pressing firmly but gently over the areas of swelling using the index finger. Edema is also a finding in problematic circulation.
- Fissures. These are dry, deep cracks in the skin, particularly on the heels, and can be a sign of neuropathy.
- Callous formation. This may indicate of an area of excessively high pressure.
- Temperature. A dermal temperature at a plantar foot location that is 2 °C (3.6 °F) or more higher than the same area on the opposite foot or than nonaffected areas on the same foot is regarded as a positive finding for inflammation; statistics show that 82% of diabetic foot ulcers are preceded by callous and inflammation (WOCN, 2022).
- Fungal infection, especially between the toes, can be attributed to poor foot hygiene.
- Bunions at the base of the great toes can indicate footwear that is too tight.
- Corns may indicate rubbing or pressure from ill-fitting shoes.
- Bony deformities can be a finding in ill-fitting footwear.
During the hands-on assessment, it is also important for the clinician to determine whether the patient can reach and see their own feet. Data show that 49% of patients with diabetic foot ulcers were unable to position their feet or see the complete surfaces of their feet. It was also found that 15% of persons with diabetic foot ulcers were legally blind in at least one eye (Baranoski & Ayello, 2020). In the event that the patient has such visual difficulties—for example, arthritic joints prevent them from seeing the bottoms of their feet—then the clinician identifies assistive devices that will allow the patient to perform proper foot checks on themself.
Over the course of one’s life, the anatomy and function of the feet change. Normal age-related changes include the fat pads on the bottom of the feet gradually becoming thinner, the arch of the foot frequently becoming flatter, and the foot becoming longer and wider. When examining the feet of patients with diabetes, the clinician distinguishes between age-related changes and changes related to diabetes.
Foot Care
Daily foot care practices for the patient with diabetes are a vital part in preventing diabetic foot ulcers from developing and are an important self-management goal. For everyone involved—patient, families, and clinicians—it is important to keep in mind that even small changes can make a big difference.
When patients understand why foot care is important, they are more likely to do it. A generalized statement that “diabetes can damage your feet” is not sufficient. The clinician does not need to go into lengthy explanations regarding the pathophysiology of diabetes. Instead, they explain that diabetes can cause two important changes that affect the feet:
- There may be a gradual loss of feeling to the feet, which the patient will not always be aware of. This can be explained to the patient in practical terms: “When you lose feeling in your feet, you may not feel a small stone or even a nail inside your shoes. You may not know that you have developed a blister or a cut on the sole of your foot. A diabetic foot ulcer can begin with something as seemingly insignificant as a small cut (nick) that happens when trimming toenails.”
- Diabetes can cause decreased blood flow to the feet. Again, the practical implications of this can be explained to the patient by stating, “Poor blood flow to your feet makes it much harder for any injury to your foot to heal, even a small wound. This can cause a small cut to turn into an ulcer.”
ELEMENTS OF GOOD FOOT CARE
- Preventing skin breakdown. The skin covering the feet provides a physiologic barrier to bacterial and fungal invasion of the tissues and bones of the feet. Skin integrity is therefore of major importance to all patients but especially to patients with diabetes, who have compromised healing (Villines, 2019).
- Maintaining the normal structure and function of the feet. This is crucial to the patient’s mobility.
- Conduct daily foot checks. Ask the patient to remove their shoes and socks and show them how to do a foot check. Every part of the foot—the tips of the toes, between the toes, the back of the heels, and the ankle areas—are to be inspected. Instruct the patient to look for red spots, blisters, cuts, swelling, and infected toenails. Many patients are unable to see the bottoms of their feet, which make foot checks difficult and can result in areas of redness being missed. In this instance, patients should be instructed in the use of a long-handled mirror to visualize all areas of their feet (Abbas & Bal, 2019).
- Wash the feet every day. Instruct the patient to wash their feet with mild soap and water. Remind patients who have a lack of sensation in their feet to check the temperature of the water with a hand before immersing their feet in order to avoid the possibility of burns. After washing, dry the feet carefully, rubbing gently to avoid chafing. Particular attention must be paid to drying between the toes, since moisture left in the web-spaces can contribute to a yeast infection. Washing the feet does not mean soaking them in water; foot soaks have been shown to break down the natural skin barrier and predispose the patient to ulcer formation (McDonald, 2019; Abbas & Bal, 2019).
- Perform skincare. Advise the patient to massage a thin coat of skin lotion onto the tops and bottoms of their feet after drying. Explain that lotion should not be put between the toes. A light dusting of talcum powder or cornstarch can be used to keep the skin between the toes dry. However, the patient must be cautioned against putting excessive powder between the toes, since this will lead to clumping and possible excoriation.
- Never walk barefoot. Most people believe that it is safe to walk in their bare feet in their own homes, and everyone has done this at some time. For a patient newly diagnosed with diabetes, it may seem nonsensical to suddenly have to wear socks and shoes (or sturdy slippers) at all times, even in their own living room. The clinician explains that inadvertently stepping on everything from a sewing needle to a sesame seed has been found to cause a diabetic foot ulcer (Abbas & Bal, 2019).
- Check shoes before putting them on. Instruct the patient to check for objects inside each shoe and to ensure that the lining of the shoe is smooth and wrinkle-free prior to putting on their shoes. Patients with small children or grandchildren, for example, have found Lego pieces and small toys in their shoes.
- Protect feet from extremes of temperature. Properly fitting shoes worn at the beach provide protection against hot sand. Also, caution the patient against using hot water bottles, electric blankets, or heating pads. Advise the patient to wear socks at night if they have cold feet. If a patient insists on wearing sandals during the summer, recommend putting sunscreen on the top of the feet to protect against sunburn.
- Improve circulation to the feet. Good circulation is fundamental to maintaining healthy feet. Teach the patient to put their feet up whenever they are sitting and not to sit for long periods of time with their feet in a dependent (dangling) position. Patients should not sit with their legs crossed for an extended time, and they should be instructed in simple exercises to do at home, such as wiggling their toes and flexing their ankles for five minutes a few times each day (McDonald, 2019). Caution the patient against wearing tight socks or elastic/rubber bands or garters around their legs to hold up stockings, as all of these can interfere with circulation.
The following elements of good foot care comprise the instructions that the clinician teaches and discusses with every patient who has diabetes and reinforces at every follow-up visit:
ANSWERING PATIENT QUESTIONS
Q:When should I check my feet, and how long is it going to take?
A:The best way to respond to this question is to have the patient demonstrate the foot check process without instructions or guidance from the clinician. This is a better indicator of the time required than simply telling the patient, “It will only take a few minutes.”
As to how frequently foot checks should be done, the clinician reinforces with the patient the need to make this part of a daily routine. A foot check can be compared to brushing one’s teeth; it is a good practice to do a foot check in the morning before putting on any footwear and again at night when the patient takes their shoes and socks off.
INDICATIONS FOR CONTACTING A HEALTHCARE PROVIDER
Patients are given clear instructions on when they should contact their healthcare provider as a result of their regular foot care. For example, “Contact your doctor’s office as soon as possible if you notice any of the following changes”:
- You start to feel pain or cramping in the legs or buttocks while you are walking or doing other physical activity
- Your feet are burning, hurting, or tingling
- You cannot feel when someone touches your foot
- You cannot tell very well whether something is hot or cold when it touches your foot
- You notice a change to the shape of your foot
- The color of your feet start to change, and they feel warmer than normal
- You begin to lose any former hair growth on your legs, feet, and toes
- The skin on your feet is dry and cracking
- The areas between your toes become red, damp, and itchy
- Toenails that were healthy and normal turn yellow and thick
- You find blisters, cuts, callouses, infected corns, or ingrown toenails on your feet
(McDonald, 2019; WOCN, 2021)
ANSWERING PATIENT QUESTIONS
Q:I have a hard callous around a small wound on the bottom of my foot. Should I cut it off myself?
A:No. Wound and foot care for a patient with diabetes should only be done by a healthcare professional. Home surgery can often cause further damage to the wound and to the foot and should be avoided.
BARRIERS TO PROPER FOOT CARE
Clinicians must remain aware of how difficult it can be for patients to make and maintain substantial changes to their lives, especially after receiving a diagnosis of diabetes. The emotional response and shock of being diagnosed with diabetes can be a major barrier for learning and self-management. This new diagnosis is something that can impact every facet of a patient’s life. Under such overwhelming circumstances, looking at one’s feet every day can seem trivial and unimportant.
It is the responsibility of the clinician to create a shame-free environment and to show respect and caring, even when it is difficult for the clinician to understand why a patient may not perform the care that they know to be important to their own well-being.
Appropriate Footwear
Proper footwear is incorporated into diabetes care from the onset of diagnosis since it is a crucial part of preventing diabetic foot ulcers. Poorly fitting shoes are frequently cited as one of the foremost causes leading to the development of diabetic foot ulcers and may contribute to around half of all diabetes-associated amputations (McDonald, 2019).
The clinician assesses the patient’s footwear at the first visit and then at regular intervals, since changes may occur in the size or shape of the patient’s foot due to edema or Charcot foot (discussed later in this course), necessitating additional adjustments and modifications to shoes (Baranoski & Ayello, 2020; WOCN, 2021).
Most everyone wants to wear nice shoes or sandals, and one of the first complaints from patients with diabetes is that specialized diabetic footwear is ungainly and ugly. At first this may seem like a trivial complaint when compared to the seriousness of developing a diabetic foot ulcer and the real potential for amputation. However, the clinician realizes that the patient is probably not thinking along those lines. Instead, they may see the loss of “normal” footwear as another unwanted indicator that a chronic disease is putting limitations on their lives. Coming from this standpoint, the clinician works with the patient in finding footwear that protects their feet but is still aesthetically pleasing to the patient. This ensures better treatment adherence on the part of the patient and better outcomes.
MEDICARE THERAPEUTIC SHOE BENEFIT
Individuals with diabetes who are at risk for foot complications and who have Medicare Part B are eligible for Medicare’s therapeutic shoe benefit. To qualify for this benefit, the person must have a diagnosis of diabetes and at least one of the following:
- History of amputation of part or all of either foot
- A previous foot ulcer or preulcerative calluses
- Peripheral neuropathy with callus development
- Diminished circulation
Each calendar year, this Medicare Part B benefit pays for:
- One pair of custom-molded shoes and inserts or one pair of extra deep shoes
- Two extra pairs of inserts for customed-molded shoes
- Three pairs of inserts for extra-depth shoes
- Shoe modifications instead of inserts
(See also “Healing Shoes” later in this course.)
(Baranoski & Ayello 2020)
ELEMENTS OF PROPER SHOE FIT
The clinician educates the patient on the importance of choosing the appropriate shoe.
The shape and size of the shoe must be assessed, and the patient advised to, as far as possible, match the shape of the shoe to the shape of the foot, both in width and length. A properly fitting shoe will have sufficient room in the toe area, over the instep, and across the ball of the foot. The shoe should fit snugly around the heel area.
A shoe with laces is a better choice for a patient with diabetes than a slip-on shoe because it provides better support and allows for adjustments needed for swelling, deformities, and different sock thicknesses (McDonald, 2019).
For patients with diabetes who have intact sensation in their feet and no evidence of foot deformities, an ideal choice is a correctly fitting pair of shoes produced from soft materials (such as soft leather) with the capacity to stretch.
Shock absorption is an important consideration for the patient with diabetes, and a cushioned sole rather than fine leather soles will provide for better shock absorption.
It is essential that shoes provide good support and protection for the feet, and the back of the shoes need to be strong enough that they will not collapse downwards or to either side, leaving the heels exposed to injury.
Ideally, patients with diabetes should have more than one pair of comfortably fitting shoes, and it is a good practice to alternate shoes on an every-other-day basis. This will help to extend the life of both pairs.
ANSWERING PATIENT QUESTIONS
Q:Will the shoes I am wearing now prevent damage to my feet?
A:This is a question that a patient will commonly ask. To answer, the clinician assesses the patient’s shoes, observing their overall condition, size, fit, and design in relation to the shape of the patient’s foot. The clinician notes the wear stress along the soles and heels and looks for thinning areas along the bottom of the shoes and the surface of the shoe lining. Are there bulges on the outside of the shoes? Excessive wearing down of the heels? Are the heels too high and too narrow?
While it may be apparent to the clinician that a patient’s shoes are not a good fit and are placing the patient at risk for developing a diabetic foot ulcer, the patient may be reluctant to accept the clinician’s findings. For instance, perhaps the shoes are relatively new and were expensive to purchase, the shoes are a favorite pair, or “they’ve never caused any problems in the past.”
Another concern is uneven weight distribution and the creation of high–pressure point areas. A quick and inexpensive way to check for this is by using a Harris mat, which is a foot imprint system. One side of the mat is permeated with ink and the other is clear. The patient is requested to remove their shoes but to leave their socks or stockings in place. The patient then takes a normal step onto the uninked side of the mat, leaving an impression of the foot on the mat that highlights areas of uneven weight distribution and high pressure (Höchste Health Care, 2020). This then allows the clinician to recommend appropriate orthotic devices to relieve pressure (or to refer the patient to an orthotist or podiatrist for further evaluation).
BUYING NEW SHOES
Patients with diabetes need to be aware of the condition of their shoes and when shoes require replacing. Signs that shoes should be replaced include:
- Heel shape that no longer provides support and collapses when the patient puts the shoes on
- Holes in the lining of the shoe
- Worn, uneven heels, which can produce an unsteady gait and/or increase the risk for excessive pressure points
- Thin, worn sole
Cost and fondness for a “worn-in” pair of shoes can make patients reluctant to purchase a new pair. The clinician must stay vigilant and point out to the patient when a new purchase is required to maintain healthy feet.
The clinician offers patients these instructions regarding purchasing shoes:
- Have your feet and proper size measured each time because feet change over time, especially with aging.
- Shop in the afternoon rather than the morning because feet swell during the day, especially if you have concomitant heart and kidney disease.
- Wear the socks (or type of socks) that you normally wear when you go to purchase new shoes. This will help to ensure that the shoes will fit properly for everyday wear.
- Measure the distance between your longest toe and the tip of the shoe. This is best done with the shoes on, pressing down on the empty space at the front of the shoe. This empty space should be one half of your thumb’s width to allow for an adequate fit.
- Break in new shoes gradually before wearing them for extended lengths of time. Wear new shoes for one to two hours, remove them, and check the feet for cuts, blisters, spots of redness, or bruising. If none of these are present, wear the shoes for 3–4 hours the following day, and each day gradually increase the wear time. If shoes are causing problems, do not “tough it out”; return the shoes to the store if the store’s return policy allows and start again with a different type of shoe.
(McDonald, 2019)
Sometimes it is hard for a patient to find the type of shoe they need “off the rack.” Clinicians can also remain aware of local shoe stores that carry footwear supplies especially for patients with diabetes and knowledgeable store staff who are able to assist a patient in choosing appropriate footwear.
COMMON FEATURES OF INAPPROPRIATE FOOTWEAR
- Seams. Seams can cause repeated shear and friction as well as pressure to the areas of the foot that they come in contact with, which are mainly the dorsal forefoot and the toes. Depending on the type of shoe, more than one seam may be present. Patients with diabetes are advised to shop for shoes that are seamless.
- Narrow toe box. A lack of space in the toe box can result in diminished circulation and increased pressure to the toes. This lack of space can result in callus and blister formation. It is important for the clinician to remind the patient with diabetic peripheral neuropathy that just because a shoe does not feel tight does not mean that it is not. The patient must carefully examine the shoe and use good visual judgment in deciding whether or not the shoe is a good fit.
- High heels. High heels can cause the development of pressure points on the balls and heels of the feet that can result in calluses and subsequent development of diabetic foot ulcers. It is recommended to wear shoes with broad, square heels that are less than 1-2 inches in height (DiLonardo, 2021).
- Insufficient length. The length of a shoe is just as important a consideration as the width. The length of the shoe should allow a 3/8- to 1/2-inch space between the patient’s longest toe and the end of the shoe (WOCN, 2022).
- Thong-style sandals and flip-flops. This type of footwear has become very popular with all age groups. However, it poses risks for patients with diabetes due to increased exposure of the foot and toes to possible injury.
SOCK SELECTION
Socks must also be considered when reviewing footwear with a patient who has diabetes. It is possible to purchase socks that are specially made for patients with diabetes in stores and from websites that specialize in diabetic supplies. For instance, compression socks, which typically indicate the degree of compression on the packaging, may be needed.
However, if the patient prefers to buy socks in “regular” stores, they are advised to avoid socks with seams that could possibly cause pressure and to look for socks that wick moisture away from the skin. Controlling moisture is very important for patients with diabetes to reduce the risk of weakening the natural skin barrier and the possibility of fungal infection.
Whether the patient is buying special diabetic socks or regular socks, the features to look for include:
- Nonelastic cuffs
- No prominent seams (turn socks inside out and run the fingers along the seams to determine how soft or coarse they are)
- Socks that keep the feet warm, especially for winter use
- Socks that allow the feet to “breathe” and sweat and that wick moisture away from the skin surfaces, particularly during the summer months
- Size (neither too tight nor sagging)
- Built-in cushioning along the bottoms for extra relief from pressure
- Light color, to alert the patient to drainage
Cotton socks absorb moisture, but they do not wick moisture away from the skin. Wool socks are usually lightweight and give good insulation; they also allow the skin to breath and absorb moisture away from the skin. Socks that are made from a mix of high-quality fibers usually provide the best wear time, comfort, and protection.
Patients should be reminded to always wear socks when they have shoes on and to change their socks every day.
Patients with diabetes often experience swelling in their lower extremities, but since most of these patients also have peripheral arterial disease, high levels of compression therapy cannot be used. However, studies have shown that mild levels of compression (18–25 mmHg) help to relieve swelling while not compromising arterial circulation (Wu et al., 2012). Thus, in patients with lower extremity swelling, the clinician discusses the value of wearing socks with mild compression.
Foot Biomechanics
Biomechanics refers to how the body moves and what impacts that movement. Two primary goals of biomechanics interventions are injury prevention and rehabilitation. Biomechanical problems can lead to an array of negative consequences on ambulation and pursuit of recreational activities as well as result in an increase in musculoskeletal comorbidities. Thus, knowledge of the biomechanics of the foot is an essential part of the assessment of the diabetic foot and an important component in preventing diabetic foot ulcers.
The gait cycle refers to one full step, beginning with either the right or left foot, from heel contact of the first foot to heel contact of the second foot. The gait cycle is further divided into the stance phase (60%), which occurs when the foot is in contact with the ground, and the swing phase (40%), which occurs when the foot is free floating.
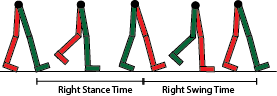
Stance and swing phases of the gate cycle. (Source: Rlawson9. Creative Commons Attribution-Share Alike 3.0.)
Proprioception refers to an awareness of the body’s position in context with the surrounding environment. Through proprioception, one knows their location in space and how to navigate through it. This functioning is accommodated by specialized nerve endings known as proprioceptors, which are found in the soft tissue of the musculoskeletal system. Next to the spinal cord, the foot is the area of the body with the most proprioceptive sensory receptors.
Damage to the feet will result when there is reduced proprioception. A lack of, or inadequate, information provided by proprioceptors has a negative impact on movement, postural coordination, and pressure (weight) distribution. In a diabetic foot with advanced neuropathy with loss of protective sensation (LOPS), diminished proprioception response is evident by unsteady gait, loss of balance, and unequal stress and weight-bearing on the feet.
When excessive weight is applied to a section of the foot, this overloading causes an overpowering, intense force that leaves no time for the skin to shield itself from injury. At this stage, blistering occurs. When there is continuous unrelieved pressure, calluses form as a protective barrier, which will eventually lead to ulcer formation.
The goal of biomechanics assessment and intervention is to assist the patient to live a healthy and active lifestyle by providing them with the education and necessary equipment to prevent injury, deformity, and the development of a diabetic foot ulcer. While being physically active plays a vital role in managing diabetes, problems with proprioception may make it difficult for patients with diabetes to be safely active. Clinicians should therefore be constantly aware of the need to maintain the patient’s activity levels while also compensating for existing deficits with ambulation and proprioception.
The first step is to ensure that the patient has good pedal support and that biomechanical issues are being addressed. This is achieved by preventing postural collapse of the foot. Research shows that custom orthotic supports also help to correct balance, gait, and structural alignment; prevent the occurrence of diabetic foot ulcers; and support treatment for ulcers already present (Zubair et al., 2021).
The clinician who sees the diabetic patient on a routine basis must be aware of the interaction between biomechanics and preserving the health of the diabetic foot. A consult with a podiatrist should happen early on in the plan of care and at least yearly thereafter. Any new problems related to ambulation and proprioception should also be referred immediately to a podiatrist (McDonald, 2019).
Addressing Foot Deformities
BUNIONS
A bunion is a protrusion, varying in size, that results from an abnormally prominent fifth metatarsal joint. Bunions can result from wearing tight-fitting, narrow shoes as well as from an inherited structural defect. During a foot exam, the clinician assesses for the presence of a bunion as a medial prominence on the side of the foot. The main treatment is to accommodate the deformity in an expanded shoe and to relieve pressure and shear that could result in wound formation (Mayo Clinic, 2020; WOCN, 2022).
HAMMERTOE
Hammertoe is a common flexion deformity of the proximal interphalangeal joint of the second, third, fourth, or fifth toes. Hammertoe deformity is also known as claw toe, since the affected toes look to be bent in the shape of a claw. It is frequently found in the second toe. Hammertoe deformity is painful and increases the risk of skin breakdown and ulcer formation.
Properly fitting footwear is the most appropriate treatment for this deformity. The clinician ensures that the front of the shoe is sufficiently high to relieve pressure from the hammertoe joints; this may necessitate a consult with the podiatrist. The clinician keeps in mind that when the toes move upward, they draw the soft tissue of the foot pad along with them, which denies the areas at the base of the toes of proper cushioning and increases the risk of callus and ulcer formation in these areas (WOCN, 2022).
CALLUSES
A callus is a thickening of the epidermis that occurs at the site of pressure on the foot. Shear and friction can also lead to callus formation. The development of a callus is seen as a protective reaction to continued stress on the affected area. Calluses should not be allowed to accumulate, as they are a common precursor to the development of diabetic foot ulcers in patients who have diabetic neuropathy. Excessive callus build-up can increase pressure to that area of the foot by 25%–35%, and this leads to the development of a diabetic ulcer beneath the callus that the clinician typically cannot see or palpate on examination (WOCN, 2022).
Discoloration of a callus or bleeding into the callus is the primary indicator of the presence of an ulcer. When examining an area of callus formation, the clinician looks closely for flecks of blood or the presence of a deeper layer of macerated, white softer tissue under the outer covering of callus. This shows the presence of an evolving ulcer and the need to immediately remove the callus tissue (Baranoski & Ayello, 2020).
The initial treatment for callus is to reduce the bulk with a scalpel while maintaining tension on the skin. Callus removal is done by a podiatrist or a clinician who has experience and training in foot care. Patchy removal of callus tissue can result in focal points of excessively high pressure and increased risk for ulcer development.
Patient education includes stressing that the patient should not attempt to remove the callus themselves (no “bathroom surgery”) and that the use of over-the-counter callus removers is not recommended, since these contain strong acids that may permit infection to gain access to the foot (WOCN, 2022).
Callus formation frequently reoccurs and requires close monitoring by the clinician. The biomechanical problem leading to the callus growth must also be addressed to obtain a permanent remedy.
Tight Glycemic Control
Tight glycemic control refers to keeping the blood sugar levels as close to normal as possible. The Diabetes Control and Complications Trial provided strong evidence that keeping blood sugar levels at or near normal levels substantially reduces the chances of developing microvascular complications of diabetes, including diabetic foot ulcers.
Poorly controlled blood sugars are a major contributing factor in the development of neuropathy in the extremities of patients with diabetes. High blood sugars also cause impaired leukocyte function, inhibit lymphocytes, and lead to an impaired immune response, which prevents the patient from mounting an adequate response to wound infection (WOCN, 2022).
The A1C test (also called the hemoglobin A1C or the glycohemoglobin test) is one of the most important tests used in diabetes management and diabetes research. The A1C test examines the binding of glucose to hemoglobin in the red blood cells. Red blood cells normally live for around three months, and by using the A1C test, it is possible to obtain an average of a patient’s blood glucose levels over the previous three months.
The A1C blood test result is stated as a percentage. The higher that percentage, the more a patient’s blood glucose levels have risen. An A1C test can be done at any time of the day and does not require the patient to have been fasting prior to the blood draw. American Diabetes Association treatment guidelines recommend that the A1C level be maintained below 7% to prevent the risk of microvascular damage in type 1 and type 2 diabetes (ADA, 2021; WOCN, 2022).
Primary care providers help patients to set reasonable goals for blood sugar levels, and this is often done in progressive increments. For a patient whose blood sugar levels have consistently remained high, getting down to the stated normal levels may seem unreasonable. However, it is essential for clinicians to provide encouragement and reiterate that any decrease in blood sugar levels helps to lessen the risk of microvascular complications occurring.
A patient may need to see their primary care provider on a monthly basis when diabetes is first diagnosed and blood sugar levels are being regulated. This also provides an excellent opportunity for ongoing education on foot care. The clinician helps the patient make the connection between blood sugar levels and foot care by explaining that high blood sugar levels cause narrowing and hardening of the arteries, which will decrease the amount of blood reaching the feet. Reinforcement of teaching, reassessment of the patient’s ability and commitment to foot care, and encouragement by the clinician are key constituents of successful outcomes.
Weight Loss
Encouraging patients to maintain a healthy weight is another facet of preventive care. According to recent data from the National Center for Health Statistics, the percentage of persons 20 years and older with obesity is 42.5%, while the percentage of those who are overweight, including obesity, is 73.6% (CDC, 2021). Being overweight plays a significant role in insulin resistance.
Patients are often doubtful about weight loss and voice fears such as, “I don’t think I can lose a whole lot.” The clinician reassures them that losing even 10 pounds can produce a considerable improvement in blood sugar levels. Most patients will agree that a 10-pound weight loss is doable, and it is then up to the clinician to help them set realistic, specific goals for a weight-loss program.
The patient is typically referred to a registered dietitian for a dietary consultation and to develop a diet program. To achieve maximum success, the diet plan takes into consideration the patient’s lifestyle, food preferences, and the fact that the patient may feel discouraged by previous failed attempts to lose weight. It is important for patients with diabetes to maintain the pleasure of eating, and this is something that the dietitian takes into consideration when assisting the patient to develop meals plans.
Follow-up with the patient is necessary to evaluate progress in meeting goals and to help resolve problems they have encountered.
Smoking Cessation
Smoking places a patient with diabetes at a very high risk for peripheral vascular diseases (in particular, peripheral arterial disease) and the development of diabetic foot ulcers. Cigarette smoking and diabetes are factors in the increased incidence of macrovascular and microvascular disease, in which both the large and small blood vessels are adversely affected. Therefore, as a preventive measure for diabetes complications, patients who smoke must clearly understand the risks of smoking and be encouraged to take part in a smoking cessation program (WOCN, 2022).
In plain language, the clinician explains to the patient that nicotine narrows the blood vessels. When there is poor circulation to the feet, the skin then becomes dry and can crack easily, and any break in the surface of the skin will potentially allow bacteria to enter and cause an ulcer to develop. Similarly, decreased circulation and oxygen delivery make it harder for an ulcer to heal.
Patients may not find it easy to give up smoking and can be highly resistant to the idea, especially after receiving a new diagnosis of diabetes, when there is a constant demand for lifestyle changes and adjustments. Many times, patients will state that they “need” to continue smoking to cope with the stress of having diabetes. The clinician recognizes this is a subject that may have to be addressed on an ongoing basis over a course of weeks or months.
Until the patient feels ready and committed to stop smoking, there is little that can be achieved. Once a patient is ready, the clinician helps them decide on a quitting strategy, such as stopping all at once, tapering off by cutting down the number of cigarettes smoked each day, using a nicotine patch, joining a smoking cessation program, or receiving acupuncture. Any of these strategies can be used singly or in combination.
Giving up smoking is not easy, and there can be frequent setbacks. Patients may be cranky and irritable, especially during the first few weeks without cigarettes. They require support and encouragement from family, friends, and the clinicians who work with them.
ANSWERING PATIENT QUESTIONS
Q:How does smoking cigarettes affect a diabetic foot ulcer?
A:Nicotine in cigarettes causes narrowing of small blood vessels. A diabetic foot ulcer requires a good blood supply to heal. Due to the narrowing of blood vessels in people who smoke, there is a diminished blood supply to the wound.
Hypertension Control
Hypertension is one of the main risk factors for the development of microvascular and macrovascular problems in patients with diabetes. Studies show that having hypertension is a strong indicator for a future diagnosis of diabetes. It has also been found that the incidence of hypertension increases considerably when diabetes is present (Tsimihodimos et al., 2018).
The patient’s blood pressure is checked with each visit, with the patient seated and having rested for approximately five minutes. Interventions used to reach target blood pressures first include lifestyle changes. Many patients are also prescribed oral medications, with the first-line recommended treatment being an ACE inhibitor taken daily (WOCN, 2022).
Recommended lifestyle modifications include:
- Weight loss
- A diet low in saturated fats and total fat content
- Restricted dietary sodium intake (no more than 2,400 mg/day)
- Regular physical exercise
- Moderate consumption of alcohol (no more than two drinks daily for males and one daily for females)
- Sufficient sleep
(CDC, 2020c)
CASE
Mr. Hernandez is a 45-year-old Hispanic man diagnosed with type 2 diabetes one month ago during a routine health check at a local clinic. At that time, he did not have a primary care provider and is being seen today for the first time by a nurse practitioner, Celia. Prior to the appointment, she reviews the patient’s chart and notes that Mr. Hernandez was started on Metformin and also has a consult for diabetes education. However, the record indicates that the patient has only attended one session with the certified diabetes educator and missed the subsequent two appointments.
Mr. Hernandez arrives for his appointment accompanied by his wife, who does not speak English. He is polite but reluctant to engage with Celia. He states that he has “no time for diabetes education” and that he is taking his medication as prescribed. He says, “My blood sugars were high because I drink too much soda.” When asked about his feet, he replies that they are fine and refuses a foot exam. Celia notes that he is wearing strong work boots and that he has no noticeable problems with his gait.
Celia acknowledges that it’s good Mr. Hernandez is having no problems with his feet and explains that this is the best time to start doing routine foot exams. She tells him that diabetes can interfere with the way the nerves in his feet work and that he can slowly lose feeling to areas of his feet without knowing it. This puts him at greater risk for injuring his feet and developing an ulcer. To compensate for the lack of feeling, daily foot checks are critical for protecting his feet from damage. Since Mr. Hernandez has refused a foot exam today, she gives him a handout on diabetic foot care and makes a note to discuss this again at his next visit.
In response to Mr. Hernandez’s statement that he has “no time for diabetes education,” Celia asks for more information about his work schedule and acknowledges that it can be hard to get time off from work to attend medical appointments. She explains that receiving diabetes education now will help lay out the best course for Mr. Hernandez to follow to control his diabetes and stay healthy, reducing the need for even more future medical appointments. She also offers to look into what other resources are available for diabetes education during the evenings or weekends.
Since Mr. Hernandez already recognizes the link between drinking too much soda and high blood sugars, Celia reinforces the need to monitor blood sugar levels and to reduce his overall sugar intake. They agree on a specific goal of reducing his current soda intake of three cans a day to one can a day, beginning the process of goal setting and gradually making the necessary lifestyle changes.
After Mr. Hernandez and his wife leave, Celia discusses his case with the physician and case manager. She explains that Mr. Hernandez does not seem to have come to terms with the fact that he has diabetes. The physician is concerned that Mr. Hernandez’s blood sugars are too high and that he is hypertensive and overweight. He requests the patient be scheduled for a follow-up appointment in four weeks. The case manager also has concerns about Mrs. Hernandez, who has previously conveyed her concern about her husband and that she doesn’t understand what is going on or what she needs to do to help him.
Together, Celia, the physician, and the case manager agree that Mr. Hernandez’s next appointment will focus on the following:
- Exploring with Mr. Hernandez his feelings about diabetes
- Including a consult with a dietitian
- Recommending a consult with a physical therapist for development of an individualized exercise program
The case manager also states that she will call Mr. Hernandez prior to the visit and get his permission to have a professional interpreter present so that his wife will know what is happening and can share her concerns.
(continues)