IMPACT OF COVID-19 ON STIs
The COVID pandemic has impacted prevention, detection, and treatment of STIs, in particular, chlamydia, gonorrhea, and syphilis, which were themselves already at epidemic levels. At the start of the COVID-19 pandemic, numerous providers cancelled nonessential in-person appointments at STI clinics, many of which provide services to high-risk and vulnerable populations, such as those without medical insurance as well as priority populations (Napoleon et al., 2020). Due to limited availability of STI testing, the actual impact of the COVID pandemic on STIs is hard to assess (Jamison & Chang, 2021).
In a survey at the start of the pandemic, the National Coalition of STD Directors found that STD services and field visits were postponed in 83% of STD clinics, and 66% of programs reported reduced screening and testing for STIs/STDs. Moreover, 57% of DISs responded that they were reassigned from STI/STD work to COVID-19 contact tracing (NCSD, 2020).
Reported cases of STDs during March and April 2020 were considerably reduced, with reported cases of chlamydia dropping to 50%, gonorrhea to 71%, and syphilis to 64% of cases compared to 2019 levels (CDC, 2021q). Three conditions that were most likely responsible for this decrease in early 2020 included reduced screening for STIs, moving STI/STD staff to COVID-19 responsibilities, and the orders to shelter in place. By the end of 2020, however, the number of reported cases of syphilis and gonorrhea once again rose (see graphic).
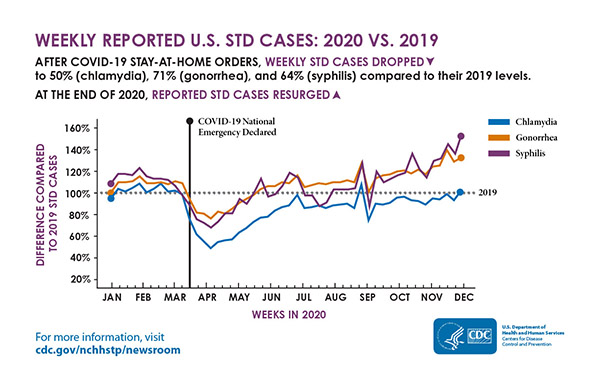
Weekly reported U.S. STD cases: 2020 vs. 2019. (Source: CDC.)
Testing for STIs has been greatly impacted by the COVID pandemic due to limited appointments, reduced hours, staffing issues, loss of finances, or closures. Some clinics moved to virtual appointments or telehealth and treated patients based on symptoms and without testing, leading providers to prescribe oral therapies, rather than intramuscular one-time treatments (Nagendra et al., 2020).
Moreover, the reagents used for STI testing of urine were being used for COVID testing, reducing the availability of this simple test leading to the need to obtain the less desirable urogenital swabs. While the patient can perform the self-swabbing, it must be done at a provider office or laboratory (Jamison & Chang, 2021). When testing is reduced, STIs go untreated.
The COVID-19 epidemic has highlighted the need for new methods of meeting the STI epidemic, including the use of telehealth, the need for self- or home-specimen collection, an increase in the use of EPT, the importance of DIS workers, and the need for other types of nontraditional treatment facilities, such as pharmacies and medical clinics in retail facilities (HHS, 2020).
SEXUAL TRANSMISSION AND COVID-19
COVID-19 is not an STI, but it can be transmitted by contact with saliva and droplets from the mouth and nose of an infected person who is in close contact. Thus far, there has been no evidence of sexual transmission of SARS-CoV-2, although the virus responsible for COVID-19 has been identified in semen and feces of infected people (NCSD and NASTAD, 2020; Tur-Kaspa et al., 2021).