PATHOPHYSIOLOGY
Coronary artery disease is the umbrella term for various syndromes of heart ischemia that are caused by atherosclerotic obstruction of the coronary arteries. The atherosclerotic damage ranges from gradual narrowing of the coronary arteries (due to bulging patches of plaque) to the obstruction of a coronary artery that can eventually lead to an MI because of the gradual narrowing of the interior diameter of the coronary arteries or the more sudden blockage of the artery(ies) by the rupture of a plaque.
Imaging technology such as a cardiac angiogram allows for the identification and quantification of the presence of atherosclerotic plaques in the coronary arteries (Virani et al., 2021).
The heart damage in coronary artery disease ranges from narrowing of a coronary artery to complete blockage of a coronary artery. (Source: National Heart, Lung, and Blood Institute.)
Atherosclerosis
Atherosclerosis is the disorder that underlies coronary artery disease. Atherosclerosis thickens the walls of medium and large arteries. The atherosclerotic thickenings occur as bulges, called plaques, in the arterial walls. Plaques contain lipids, white cells, smooth muscle cells, and connective tissue in a poorly organized mass that lies just under the endothelial lining of the artery wall.
The atherosclerotic plaques combine with inflammation and scar tissue to exacerbate partial or complete blockage of the coronary arteries, causing myocardial ischemia or infarction. When atherosclerosis affects the coronary arteries, the problem is usually systemic as well. Occlusions may occur in large or small arteries, compromising circulation (Virani et al., 2021).
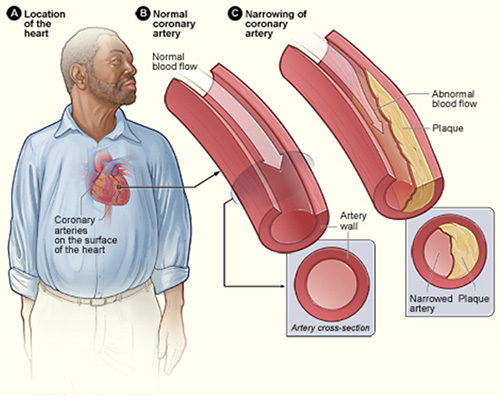
In atherosclerosis, fat and cells collect in bulges just below the surface of the lining of arteries. These bulges are called plaques. Over time, the plaques thicken and reduce the inner diameter of the arteries, allowing less blood to get to tissues beyond the plaques. (Source: National Heart, Lung, and Blood Institute.)
In the United States, atherosclerosis usually begins in childhood or adolescence and then gradually worsens over many decades. Children as young as 2 years have been found to have atherosclerotic plaques throughout their arteries. Childhood obesity and diabetes contribute to this.
Any medium or large artery in the body can be affected. Most atherosclerosis causes no clinical problems. Many people have atherosclerosis throughout their bodies but develop no serious medical symptoms and the disease is only discovered at autopsy. This is referred to as subclinical atherosclerosis.
When atherosclerosis causes the coronary arteries to become very narrow or when plaques rupture and send clots into the arteries of the heart, a person is said to have CAD.
When the effects of atherosclerosis reduce the circulation in noncardiac arteries, a person can develop peripheral artery disease (PAD).
- In the carotid arteries, PAD can cause strokes.
- In the legs, it can cause episodic pain when walking (intermittent claudication) and sometimes gangrene of the feet.
- In the gastrointestinal arteries, it can cause mesenteric ischemia.
- In the renal arteries, it can cause stenosis leading to hypertension or renal failure.
ATHEROSCLEROTIC PLAQUE FORMATION
Atherosclerosis is characterized by the formation of atherosclerotic plaques formed primarily of lipid deposits, which develop slowly over many years and in three stages.
Stage One: Fatty Streaks Appear
As atherosclerosis begins, the first detectable changes are the appearance of fatty streaks along artery walls, typically observed via CT scan or cardiac catheterization. These streaks are places where excess fat is accumulating.
Most of the fat (lipids) in the blood is carried by proteins in molecular complexes called lipoproteins. The surface of a lipoprotein is made of the more water-soluble lipids (cholesterol and phospholipids). The least soluble lipids (cholesteryl esters and triglycerides) are carried in the centers of the lipoproteins.
Lipoproteins are found in five sizes. From the largest to the smallest, these are: chylomicrons, VLDL, IDL, LDL, and HDL. Each size lipoprotein has its own characteristic balance of lipids. The largest lipoproteins (chylomicrons and VLDL) are especially rich in triglycerides, while 70% of all blood cholesterol is contained in the LDL lipoproteins. Treatment that lowers LDL cholesterol levels may reverse the process that causes fatty streak formation.
When there is an excess of lipoproteins in the blood, as happens in hypercholesterolemia, more lipoproteins than normal get through the endothelial cells and into the artery walls. These excess lipoproteins stick to extracellular molecules, and eventually enough excess fat becomes stuck just below the endothelial cells to form visible yellowish (fatty) streaks along the arterial walls. These may develop as early as the age of 20 and involve progressively greater areas of the tunica intima of the interior of arteries as people age.
Stage Two: Fibrous Plaque
With injury to the epithelial lining of the arterial wall, smooth muscle cells move into the fatty plaques and cause arterial thickening. Collagen covers the fatty streak and forms a fibrous plaque that is greyish white. Lipoproteins move cholesterol and other lipids into the tunica intima of the arterial wall. White blood cells are also attracted to the lipids, causing the plaque to grow larger. The result is further narrowing of the opening or lumen of the artery, reducing and slowing the flow of blood. Progressive changes in the artery wall can begin as early as age 30.
Stage Three: Complicated Lesion
As the fibrous plaque continues to grow, inflammation can occur. Inflammation is the proliferation of white blood cells (WBCs) that respond to fight what the body perceives as an invader. Any interruption in the smooth inner wall of the artery is seen as an invader. This may cause the plaque to become unstable, causing it to rupture or leading to an ulceration or lesion.
When atherosclerotic plaque formation triggers an inflammation response, WBCs (particularly lymphocytes and macrophages) collect under the epithelial cells in the arterial wall and release inflammatory molecules, cytokines, and proteolytic enzymes. As they continue to evolve, some plaques also accumulate calcium, which can sometimes be seen in X-rays.
In time, the endothelial cells covering the bulge begin to rip, letting blood come in contact with the underlying collagen and other extracellular molecules. Extracellular molecules are stimulants of blood clotting. Therefore, small blood clots and clumps of platelets form along the rips in the endothelial lining of the artery. Disrupted plaques create blood clots, and if the clots break loose, they are carried into the smaller arteries downstream. The result can be a blocked artery (Lewis et al., 2020; Sole et al., 2021).
CLOTS AND VASOSPASMS
The rupture of a plaque can also cause the walls of the artery to constrict in that region. The resulting vasospasm narrows the artery suddenly and causes ischemia downstream. Alone and together, clots and vasospasms can cause emergency medical conditions, including heart attacks and sudden death. A coronary artery vasospasm occurs at rest, responds to nitrates, and occurs in the presence of normal diagnostic tests such as a chest X-ray, electrocardiogram, and serum troponin levels (Lewis et al., 2020; Sole et al., 2021).
The rupture of an atherosclerotic plaque can happen quickly. It can be set off by a sudden spurt of output from the sympathetic nervous system. Such spurts can occur when people are waking in the morning or when people are subjected to strong emotional stress. External stresses, however, do not disrupt stable plaques. External stresses only rupture those plaques that have already become weakened and destabilized by inflammation or other internal changes.
ATHEROSCLEROSIS OF THE CORONARY ARTERIES
Rather than uniformly thickening arterial walls, atherosclerosis is patchy and unevenly distributed. The specific coronary arteries affected by atherosclerosis vary from person to person, but there is a common feature: within a coronary artery, plaques are found most often at branch points, places where the blood flow naturally becomes turbulent.
The narrowing of coronary arteries usually occurs slowly, and in response, new small collateral arteries have time to grow into the fields of the atherosclerotic arteries to help bolster the local oxygen supply. These collateral arteries will sometimes provide enough extra blood flow to keep the heart muscle working comfortably at a resting rate. The collateral arteries are small, however, and they do not have the capacity to keep up with the oxygen demands of heart muscle during exercise.
Even with the growth of small collateral arteries, the continual narrowing of the coronary arteries by atherosclerosis can eventually produce ischemia and anginal pain. Initially, these symptoms occur only when the patient is exercising; later, the symptoms begin to occur even when the patient is at rest.
Besides slowly narrowing the coronary arteries, atherosclerosis can cause a sudden medical crisis. The degeneration of a plaque can seed clots into the bloodstream and can also trigger local vasospasm. These lead to a marked reduction of blood flow, and the resulting damage can range from temporary to permanent and from mild to fatal.
CAUSES AND CONTRIBUTORS
There are several causative factors that contribute to the formation of atherosclerosis in the arteries. Some people have a genetic propensity for developing atherosclerosis, but it appears that the disease can occur in almost everyone. Contributing factors can increase the extent of atherosclerosis and the possibility that the condition will be symptomatic.
- There is a prevalence of atherosclerotic formation in families with higher episodes of cardiac incidents.
- Nutritional intake of trans fats and lipids contributes to atherosclerosis.
- The use of tobacco in any form causes vasoconstriction that will increase arterial wall tension.
- Physical inactivity prevents a person from obtaining the benefits of exercise, such as weight and blood pressure reduction and the development of collateral circulation.
- Obesity is associated with subclinical atherosclerosis, including coronary artery calcification and carotid intima-media thickness.
- High blood levels of LDL and lipids contribute to the production and size of arterial wall plaques.
- The development of atherosclerotic plaques are progressive and worsen as a person ages.
(Virani et al., 2021)