CIRCULATION OF THE HEART
The heart is made up almost entirely of muscle. Cardiac muscle, which differs from the skeletal and smooth muscle of the rest of the body, is dependent on aerobic metabolism. This means that the heart cannot function without a constant supply of oxygen.
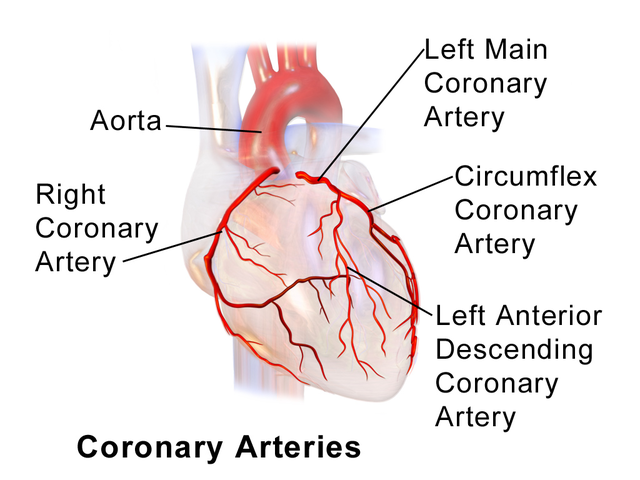
The coronary arteries and their main branches are large, and they run along the outer surface of the heart. The smaller arteries, which directly feed the heart muscle, dive deep into the walls of the heart. (Source: BruceBlaus, Creative Commons Attribution 3.0.)
Coronary Arteries
Just beyond the aortic valve—the outflow valve of the left ventricle of the heart—the right and left coronary arteries are the first branches of the aorta. The two coronary arteries and their main branches run in grooves along the outside of the heart; these grooves separate the left and right ventricles, and they also separate the atria from the ventricles. The coronary arteries and their main branches are called epicardial arteries because they run on the outer surface of the heart.
From the coronary arteries and their major branches, many small arteries run into the muscular walls of the heart, and these small arteries give rise to rich capillary networks that bathe the cardiac muscle cells with blood and oxygen during diastole. All arteries inside the heart walls are fed by branches of either the right or left main coronary arteries.
People may vary in the way the blood supply to the heart is divided between the right and left coronary arteries due to anatomical differences. In most people, the left coronary artery supplies most of the blood used by the left ventricle, the interventricular septum, and part of the right ventricle. The right coronary artery supplies most of the blood used by the walls of the right ventricle and part of the posterior wall of the left ventricle. In 90% of people, the right coronary also supplies the atrioventricular (AV) node and the bundle of His, causing serious dysrhythmias in the presence of blockage.
There is not much overlap between the territories of the major branches of the coronary arteries. Therefore, if one of the major branches suddenly becomes blocked, there is no other blood supply to the territory served by that branch, and muscle in that territory will be deprived of oxygen (Lewis et al., 2020).
A common finding in coronary artery disease is collateral circulation, the development of additional arteries that form a natural bypass from one side of a blocked artery to the other. Research suggests that coronary collateral circulation may help to improve angina, reduce ischemia, preserve ventricular contractile function, and improve prognosis in patients with coronary artery disease. Collateral circulation may be increased by physical exercise (Cleveland Clinic, 2019).
LEFT CORONARY ARTERY
The left coronary artery splits into two main branches, the left anterior descending (LAD) coronary artery and the left circumflex coronary artery. The LAD coronary artery runs down the front of the heart along the groove between the left and right ventricles. In most people, the LAD supplies blood to the front wall of the left ventricle and to the interventricular septum. Loss of blood flow to the left ventricle causes infarcted tissue that will compromise the ventricle’s ability to pump blood to rest of the body. Forty to 50% percent of MIs are caused by an obstruction of LAD coronary artery.
The left circumflex coronary artery runs to the left (at a right angle to the LAD) along the groove between the left atrium and the left ventricle. The left circumflex coronary artery supplies blood to the side or lateral wall of the left ventricle. Fifteen to 20% of MIs are caused by an obstruction of the left circumflex coronary artery (Lewis et al., 2020).
RIGHT CORONARY ARTERY
The right coronary artery (RCA) runs to the right, along the groove between the right atrium and the right ventricle. The RCA branches behind the heart and gives rise to the posterior descending coronary artery, which parallels the LAD in front. The RCA supplies the apex and the posterior of the heart. In most people, it supplies blood to the right ventricle and to the sinus and AV nodes of the heart’s electrical conduction system. Thirty to 40% of heart attacks are caused by an obstruction of the RCA (Lewis et al., 2020).
Normal Blood Flow to the Heart
The blood flow through the heart usually keeps up with the body’s demand. The demand is increased by exercise and strong emotions, both of which make the heart pump more quickly and more forcefully, causing the heart to use more oxygen. When the heart beats twice as fast, it needs twice as much oxygen. Increased cardiac workload leads to increased oxygen demand. Normally, the extra oxygen needed during exercise is supplied by a faster and more voluminous blood flow through the coronary arteries.
HEART RATE
Faster blood flow is a direct result of a faster heart rate. Blood flow to the heart automatically speeds up as the heart beats more quickly because the coronary arteries are fed directly by the outflow of the aorta (Lewis et al., 2020).
ARTERIAL WALL TENSION
Throughout the body, the volume of blood flow is regulated by the size of the arteries. Arteries have an innate tension in their walls. This tension keeps arterial volume at a particular level, and the tension also creates a resistance to blood flow. When the arterial wall tension is reduced, the artery stretches more easily and can carry a larger volume of blood.
The natural state of coronary arteries and their main branches is relatively wide open, and in general, these arteries do not limit the volume of blood getting to the muscle cells inside the heart. Instead, it is the small arteries inside the walls of the heart that widen and narrow, thus controlling the volume of blood flow to the muscle cells.
The control of the arterial wall tension (the force that widens and narrows the arteries) is local. As muscle cells work harder, they change the concentration of molecules (e.g., oxygen) surrounding them. Most molecular changes resulting from hard work relax the arteries in the vicinity. In addition, during exercise or stress, sympathetic nerves reduce the tension in the walls of arteries. Together, these factors relax the walls of the arteries and increase the local blood flow.
In older adults, the arteries become progressively stiffer with aging. This causes displacement of the arterial wall, especially when exacerbated by hypertension or other comorbidities, which can put the person at higher risk for atherosclerosis (Lewis et al., 2020).
Myocardial Ischemia
Myocardial ischemia occurs when blood flow and blood volume are insufficient to supply all the oxygen needed by the heart muscle.
BLOOD LOSS TO MUSCLE CELLS
What happens to heart muscle cells when they become ischemic? As soon as the blood flow to an area of heart muscle is stopped, the cells begin to lose their energy stores, and within a few minutes the muscle cells are no longer able to contract. Any region of the heart that loses all its blood flow will stop working almost immediately.
Although muscle cells stop working, they do not begin to die until 20 to 30 minutes after losing their blood supply. This is because the tissues remain at least partially oxygenated for a brief period until the lack of new or insufficient blood supply causes irreversible tissue necrosis. If blood flow is restored within a half hour, most muscle cells will eventually recover; however, the recovery can take from 10 minutes to several days. During that time, the heart acts “stunned” and may not contract well unless stimulated by inotropic drugs (Ecgwaves, 2018).
Another effect of sudden ischemia of the heart is electrical irregularity. Before muscle cells begin to die, they become electrically unstable. After the blockage of a major coronary artery, the electrical instability of some people’s hearts may lead to ventricular fibrillation. This is potentially fatal.
SYMPTOMS OF ISCHEMIA
Cardiac ischemia usually produces symptoms, and the classic symptom of reduced oxygen supply to the myocardium is a type of chest pain called angina pectoris, or simply angina. Angina, from the Latin word that means “squeezing,” typically feels like crushing or squeezing, although sometimes it is described as burning or pressure. The sensation is usually felt inside the chest behind or just to the left of the sternum. The feeling can also radiate to the lower part of the neck, jaw, shoulder, back, or down the ulnar side (inside) of the left arm. The feeling can radiate to either or both arms.
The sensation of angina can vary from mild to diffuse unbearable pain. It is transient and does not cause cell damage but may be a precursor to the tissue death that will occur if the ischemia that causes angina is not treated and progresses to an MI. Other symptoms that may accompany the chest pain include nausea, dyspnea, fatigue, and dyspepsia (Sole et al., 2021).
Although women tend to visit their physicians more often than men and therefore report more symptoms, including chest pain, their angina symptoms usually present in the form of upper abdominal discomfort, neck or jaw pain, or shortness of breath as opposed to crushing or squeezing chest pain. Women are also more likely than men to associate their angina with emotional or mental stress. Both the American Heart Association and the Centers for Disease Control and Prevention recommend that women be educated on gender-specific symptomology to ensure that diagnostic procedures and treatment start within one hour of cardiac-based symptoms (CDC, 2020a).
Chronic Stable Angina
Chest pain that occurs over a long period of time that exhibits similar onset, duration, and intensity is referred to as chronic stable angina. It may be caused by exertion, stress, or negative emotions. Rather than pain, the symptoms may be described as pressure, tightness, heaviness, burning, squeezing, or discomfort in the chest. The person may also describe experiencing dyspnea or fatigue at the same time. The pain may radiate to the jaw, neck, shoulders, or arms. The complaint usually only lasts a few minutes. The pain is usually relieved by resting or taking a nitrate such as sublingual (sl) nitroglycerin (NTG). This form of angina may progress to unstable angina.
Unstable Angina
This form of angina is newly occurring with a duration of 10 minutes or more. It may occur at rest with no precipitating factors. It is considered much more dangerous than chronic stable angina and requires immediate treatment. It may not be relieved by rest or nitrates. It may be accompanied by fatigue, nausea, dyspnea, or anxiety. Fatigue is the most common concurrent symptom. This form of angina may progress to an MI.
Prinzmetal’s Angina
This is a rare type of angina that often occurs at rest. It is more common in those with a history of migraine headaches, Reynaud’s disease, alcohol consumption, cocaine usage, or heavy smoking. The most common cause of this angina is not necessarily related to CAD but is usually caused by the spasm of a coronary artery resulting in a temporary loss of oxygenated blood to the related area of the myocardium. The pain may be accompanied by a transient episode of ST-segment elevation, indicating hypoxia, and occurs in short bursts at approximately the same time each day. The spasm occurs during a period of increased oxygen demand such as rapid eye movement (REM) sleep or exposure to cold. The pain may subside in response to moderate exercise or sl NTG. Supplemental oxygen may help relieve the pain if administered while hypoxia is occurring.
Microvascular Angina
In this type of angina, the myocardial ischemia is caused by atherosclerosis or spasm of the distal branches of the coronary artery branches and microcirculation, rather than the actual coronary arteries. This is also known as coronary microvascular disease (MVD) or Syndrome X. It is more common in postmenopausal women, may be very prolonged, and is often caused by physical exertion. Angina caused by arteriospasm is often fleeting, and the diagnosis is made by ruling out any other anatomical cause. The response to nitrates is intermittent. Supplemental oxygen may help relieve the pain if administered while hypoxia is occurring (Johns Hopkins, 2021).
Takotsubo Cardiomyopathy
This form of angina is also known as stress cardiomyopathy or “broken heart syndrome.” Accompanying the chest pain is ST-segment elevation, mild cardiac biomarker (e.g., serum troponin) elevation, but no coronary artery narrowing. It is named for the Japanese trap used to capture an octopus. In the presence of stress hormones (as in the case of a “broken heart”), the cardiac muscle will temporarily bulge at the apex, resembling the same shape as an octopus trap. The pain is caused by a temporary decrease in blood flow through the coronary arteries, as in CAD. The pain may not be severe enough to require supplemental oxygen (Harvard Health Publishing, 2020).
Dysrhythmias
Another significant result of sudden ischemia is a change in the heart’s rhythm. Such changes can be serious. The arrhythmias (notably, ventricular fibrillation or ventricular tachycardia) that sometimes result from heart ischemia are the most common causes of sudden cardiac deaths after an acute myocardial infarction.