ASTHMA TREATMENT
The goals of treatment for asthma include:
- Preventing long-term symptoms that interfere with daily living
- Maintaining lung function near the person’s personal best measurement
- Preventing repeated asthma attacks
- Providing the best medical treatment with the fewest possible side effects
Drugs are the cornerstones of asthma therapy, and patients with asthma typically take at least one medication daily. Asthma therapy with medications has two modes:
- Short-term treatment of asthma attacks with quick-relievers (rescue medications)
- Long-term treatment of the disease to minimize attacks and to moderate symptoms with daily controllers
The routes of delivery for asthma medications are systemic (oral or injectable) and inhaled. The inhaled route is more convenient and is used most commonly because of fewer side effects and quicker onset of action.
There are four types of asthma medicines and treatments:
- Quick-relief medicines that work quickly and are taken as needed at the first sign of symptoms
- Controller medicines that treat asthma by correcting the underlying changes in the airways, such as swelling and mucus hypersecretion; can be combined with other medications
- Combination of quick-relief and controller medicines used for both short-term relief and control
- Biologics given by injection or infusion to target a cell or protein to prevent swelling inside the airways, used for certain types of persistent asthma
(AAFA, 2021g)
Drug Administration: Inhalation
Many asthma drugs are administered by inhalation to send the medication directly to the target tissue, the inner linings of the airways of the lung. Higher concentrations of medicine can be delivered this way with fewer systemic side effects.
TYPES OF AEROSOL DEVICES
A variety of devices are available for delivering drugs directly into the lungs. The common aerosol devices are described below.
Nebulizer
A nebulizer is a drug delivery device used to change medication from a liquid to a mist so that it can be more easily inhaled into the lungs through a mouthpiece or mask worn over the nose and mouth. A nebulizer is the most common device used to deliver medications to infants, small children, and patients requiring hospitalization.
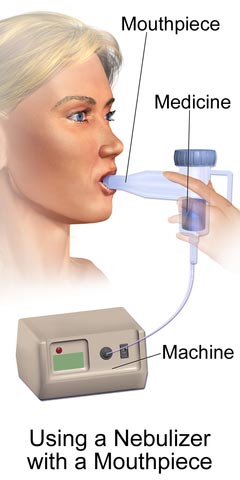
(Source: BruceBlaus, CC SA 4.0 International.)
Metered-Dose Inhaler (MDI)
An MDI is a pressurized canister containing medication that fits into a boot-shaped mouthpiece. The canister is activated by compressing it into the boot, which delivers a metered dose of the drug to be inhaled. This is the most common device used to deliver medications in an ambulatory setting.

Metered-dose inhaler (MDI). (Source: NIAID, CC 2.0 Generic.)
Spacers, or valved holding chambers (VHCs), are often used with non-breath-activated MDIs to minimize local side effects and enhance drug delivery. A spacer is a simple tube added to the mouthpiece of an MDI to move the inhaler farther from the patient’s mouth. A VHC is a spacer with a one-way valve that keeps the patient from exhaling into the MDI.

Child using inhaler with spacer. (Source: Michael J. Ermarth, FDA.)
Dry Powder Inhaler (DPI)
This device that does not use a chemical propellant to push the medication out of the inhaler. Instead, the medication is released through the mouthpiece by deep and fast inspiration. A DPI is not indicated for use in children younger than 12 years because of the requirement of a high inspiratory flow.

Dry powder inhalers (left to right): Turbuhaler, Accuhaler, Ellipta devices. (Source: NIAID, CC SA 4.0 International.)
Soft Mist Inhaler (SMI)
A soft mist inhaler is a newer type of device that creates a cloud of medicine that is inhaled without the assist of a propellant. Because the mist contains more particles than MDIs and DPIs and the spray leaves the inhaler more slowly, more of the drug enters the lungs (Hess & Dhand, 2020).
PROPER USE OF INHALERS
It is important to read the device-specific instructions for proper use of any inhaler if it is to be effective. The following are general instructions for use of inhalers.
Most asthma patients use MDIs for their quick-relief medications. It is easiest to learn the proper use of an MDI through an in-person demonstration. All patients who are prescribed medications using inhalers should receive initial instructions and careful follow-up to ensure proper use. These are the essential steps whether or not a spacer or VHC is used:
- Take the cap off, inspect to make certain mouthpiece and spray hole are clean, and shake the inhaler 10 to 15 times.

- Take a breath in and fully exhale the air in the lungs.

- Hold the inhaler upright with finger on the top of the canister and thumb holding the bottom of the inhaler.

- Put the inhaler in the mouth above the tongue and between the teeth. Seal lips around the inhaler. Close the lips around the mouthpiece (closed-mouth technique) or hold the mouthpiece 1 to 2 inches in front of the open mouth.

- Begin to breathe in slowly. Press down on the inhaler one time and keep breathing in. (If the inhaler has a spacer or holding chamber, press down on the inhaler and wait 5 seconds before beginning to inhale.)

- Hold the breath for 5 to 10 seconds.

- Open the mouth and breathe out slowly.

(Source: CDC, 2018.)
If taking 2 puffs of the quick-relief medication, wait 15 to 30 seconds and shake the inhaler again before taking the second puff. For other medicines it is not necessary to wait before taking the prescribed number of puffs. If using a steroid inhaler, rinse the mouth with water, gargle, and spit out the water (Hess & Dhand, 2020).
When using a dry powder inhaler, the steps are the same; however, the inhaler is activated when the person inhales, not by pressing down on a tube.
INHALER CLEANING
It is important to keep the inhaler clean. Any powder in or around the hole where the medicine sprays out should be cleaned.
- Remove the metal canister from the L-shaped plastic mouthpiece. Do not wash the canister or immerse it in water.
- Rinse only the mouthpiece and cap by running warm tap water through them for 30–60 seconds.
- Shake off excess water and allow the mouthpiece and cap to air dry overnight.
- In the morning, put the canister back inside. Put the cap on.
- Replace the mouthpiece cover.
- If it is necessary to use the inhaler before the mouthpiece is dry, shake off excess water, replace canister, and test spray two times (away from the face).
- Follow the manufacturer’s instructions for cleaning a dry powder inhaler.
(Hess & Dhand, 2020)
INHALER MISUSE
A study of patients from adult and pediatric clinics has shown that up to 92% of individuals with asthma do not use inhalers correctly, and problems are not limited to only one type of device. This study showed that even among medical personnel, rates of correct use are suboptimal. Another study found that 1 in 4 patients had never received instructions on proper inhaler technique. It is obvious, therefore, that improving techniques will improve clinical outcomes (AAFA, 2019b; Makhinova et al., 2020).
For MDI users, the most common errors involve coordination, speed and/or depth of inspiration, and postinhalation breath-hold. The most common errors among dry-powder inhaler users were incorrect preparation, no full expiration after inhalation, and no postinhalation breath-hold.
Incorrect inhaler technique is linked to a significantly greater risk for inhaled corticosteroid overuse. Unintentional nonadherence to first-line rescue inhalers can lead to use of long-acting inhaled medications that might not otherwise be needed. Improper use of inhaled corticosteroids can increase the risk of pneumonia and other direct and indirect complications. These findings highlight the importance of inhaler technique training.
The gold standard for teaching inhaler technique is Teach-To-Goal (TTG), which combines assessment and education through rounds of demonstration and patient teach-back. Teach-back has been associated with a statistically significant improvement in inhaler use and may require multiple sessions to ensure skills are retained (Rodriguez, 2019a).
CASE
Inhaler Education
Kamiko is a 35-year-old woman who has recently been diagnosed with asthma and has returned for her second follow-up appointment. She has an appointment with the office nurse to receive additional education on controlling her disease. During the visit her medications are discussed and reviewed, as well as the new asthma action plan developed between herself and her primary care physician.
When Kamiko was newly diagnosed with asthma and prescribed a rescue inhaler, she was given training in the proper use of the inhaler using the Teach-To-Goal technique and was able to demonstrate proper technique and understanding of care of the device.
Today before Kamiko leaves the office, the nurse asks her to demonstrate the use of her inhaler again. A dummy inhaler is provided, and as the nurse watches, Kamiko proceeds through the steps.
Following her demonstration, the nurse points out three problems with Kamiko’s technique. First, she did not fully exhale all the air in her lungs before inhaling the medication. Secondly, she did not shake the inhaler again before administering a second dose. And lastly, she did not begin to inhale until she had sprayed the medicine into her mouth.
The nurse next demonstrates the proper technique for Kamiko, who then returns the demonstration, showing that she can now use her inhaler correctly. She is given a pamphlet to refer to at home that visually guides her through the technique, and another follow-up appointment is made with the nurse for reevaluation in two weeks.
Bronchodilators
Bronchodilators are used to reverse the bronchoconstriction of asthma attacks and in this way to relieve cough, wheezing, dyspnea, and chest tightness. Bronchodilators are also the primary medicine for preventing exercise-induced bronchoconstriction. There are three classes of bronchodilators:
- Beta-2 agonists
- Anticholinergics
- Methylxanthines
SHORT-ACTING BETA-2 AGONISTS (SABAs)
Short-acting beta-2 agonists are often referred to as “quick-relief” or “rescue” medications. The smooth muscle in bronchioles (small airways) is relaxed by beta-2 adrenergic agonist drugs, reversing and preventing further contraction of muscle cells.
Because beta-2 agonists have a wide array of effects throughout the body, they are preferably administered by inhalation directly to the inner lining of the airways. When inhaled, they produce an effect in less than 5 minutes and the effect then lasts for 2–4 hours.
| Generic Name | Brand Name |
|---|---|
| Albuterol | Proventil HFA Ventolin HFA Proair HFA Proair Respiclick Proair Digihaler AccuNeb solution |
| Levalbuterol | Xopenex Xopenex HFA Levalbuterol HFA |
| Terbutaline (oral) | None |
Side effects:
- Tachycardia
- Tremors
- Jitteriness
- Palpitations
Precautions:
- Patients with heart disease, hyperthyroidism, seizure disorder, or hypertension should be closely monitored
(AAAI, 2021)
LONG-ACTING BETA-2 AGONISTS (LABAs)
LABAs are recommended for use only in conjunction with inhaled steroids in asthma. Long-acting bronchodilators are used to provide control, not quick relief of asthma. They should only be used with inhaled steroids for long-term control of asthma symptoms (AAAI, 2021).
| Generic Name | Brand Name |
|---|---|
| Formoterol fumarate inhalation powder | Foradil |
| Salmeterol | Serevent Diskus |
| Oldodaterol | Striverdi Respimat |
ANTICHOLINERGICS
Another group of bronchodilators, anticholinergics, are muscarinic receptor antagonists (parasympatholytics). They are used along with beta-2 agonists for treatment of severe symptoms. They are not, however, intended for acute asthma attacks.
Whereas beta-2 agonists affect the bronchioles (small airways), anticholinergics affect the muscles around the bronchi (large airways) by blocking receptors that cause spasm and by decreasing secretion of mucus. Anticholinergics begin to work within 15 minutes, work best after 1 to 2 hours, and usually last from 3 to 4 hours or up to 6 hours in some people.
| Generic Name | Brand Name |
|---|---|
| Ipratropium bromide | Atrovent HFA |
| Long-acting tiotropium | Spiriva Respimat |
| Umeclidinium | Anora Ellipta Incruse Ellipta |
Side effects:
- Dry mouth
Precautions:
- Individuals with glaucoma should be carefully monitored by an ophthalmologist.
- Persons with allergy to soya lecithin (e.g., soybeans, peanuts) should not take these drugs.
(AAFA, 2021h; Schiffman, 2020; FDA, 2021b)
METHYLXANTHINES
Methylxanthines belong to the class of bronchodilators that includes caffeine. These drugs have two distinct effects in the airways: smooth muscle relaxation and suppression of the response of airways to stimuli. They also have an effect on mucus clearance. Methylxanthines can be helpful for relief of nighttime asthma symptoms.
Theophylline is an alternative, but not preferred, therapy in mild to moderate persistent asthma. It is usually reserved as an add-on or third-line therapy, most often in combination with inhaled therapy, and its use requires monitoring of plasma concentrations so that therapeutic but not toxic levels are achieved.
Aminophylline is a combination of theophylline and ethylenediamine in a 2:1 ratio. This medication is used as a second- or third-line adjunct treatment for asthma (ethylenediamine is an additive that increases pH sufficiently enough to dissolve theophylline).
| Generic Name | Brand Name |
|---|---|
| Theophylline (short-acting) | Elixophyllin Theochron |
| Theophylline (long-acting) | Theo-24 |
| Theophylline and dextrose injectable | None |
| Aminophylline (injectable) | None |
Methylxanthines have a narrow therapeutic range and thus a high incidence of adverse effects.
Mild side effects:
- Nausea and vomiting
- Increased gastric acid secretion and subsequent GERD
- Polyuria
- Insomnia
- Palpitations
- Headache
- Tremors
- Weakness
Severe side effects:
- Intractable vomiting
- Arrhythmias
- Tachycardia or bradycardia
- Cardiac arrest
- Allergic skin reactions
- Seizures
Precautions:
- Because theophylline is related to caffeine, ingesting large amounts of caffeine in coffee, tea, chocolate, or soft drinks may increase theophylline side effects.
- Some drugs, such as cimetidine (Tagamet), erythromycin (E.E.S.), and ciprofloxacin (Cipro), may increase theophylline levels.
- Certain diets, such as high-protein/low-carbohydrate or vice versa, may change the effect of theophylline.
- Phenytoin (Dilantin) and carbamazepine (Tegretol) may decrease theophylline levels.
Contraindicated for people with the following:
- Cardiovascular disease
- Cystic fibrosis
- Hepatic impairment
- Hypo or hyperthyroidism
- Peptic ulcer disease
- Seizure disorder
- Pregnancy and breast feeding
(FDA, 2021b; Gottwalt & Tadi, 2021)
Corticosteroids
Corticosteroids are variants of the natural hormone cortisol. Corticosteroids dampen inflammation at the level of cell nuclei, switching off genes for inflammatory molecules such as cytokines, chemokines, and inflammatory enzymes, and activating genes that have anti-inflammatory effects.
INHALED CORTICOSTEROIDS
Inhaled corticosteroids (ICSs) are considered the most potent and consistent anti-inflammatory agents currently available for preventing exacerbations in patients with persistent asthma. Regular use of these medications reduces the frequency of asthma symptoms, bronchial hyper-responsiveness, and risk of serious exacerbation, and improves quality of life.
ICSs work directly at the cellular level by reversing capillary permeability and lysosomal stabilization to reduce inflammation. The onset of action is gradual and may take from several days to several weeks for maximal benefit with consistent use. Recently updated guidelines recommend ICSs be used for acute asthma symptoms in conjunction with beta-2 agonists in adolescents and adults.
ICSs come in liquid capsule formulation given through a nebulizer machine, metered-dose inhalers (MDIs) administered through spacers, and dry powder inhalers (DPIs). These medications are initiated in a stepwise fashion based on the frequency and severity of asthma symptoms. Low-, medium-, and high-dose inhaled corticoids are available to treat mild, moderate, and severe persistent asthma (Liang & Chao, 2021).
| Generic Name | Brand Name |
|---|---|
| Beclomethasone dipropionate | QVAR Redihaler* |
| Budesonide | Pulmicort Flexhaler Pulmicort Respules |
| Fluticasone propionate | Flovent HFA Flovent Diskus Advair HFA+ Arnuity Ellipta Armonair Digihaler Armonair Respiclick |
| Mometasone | Asmanex HFA Asmanex Twisthaler |
| Ciclesonide | Alvlesco |
| *QVAR Redihaler is the first and only breath-actuated aerosol inhaled corticosteroid for use in patients 4 years of age and older. |
|
Side effects:
- Mouth and throat irritation
- Dysphonia
- Oral yeast infections
- Reflex cough
- Bronchospasm
- Risk of bone fractures with high doses
Precautions:
- ICSs may decrease growth in children, so the lowest dose possible should be prescribed.
- ICSs may increase risk of serious or fatal infections in those exposed to serious viral infections (e.g., chickenpox, measles).
- ICSs can cause cataracts or glaucoma.
- ICSs can increase the risk of pneumonia.
- Symptomatic patients on long-term, high-dose ICS should be screened for:
- Cataracts
- Glaucoma
- Hypothalamic-pituitary-adrenal axis dysfunction
- Impaired glucose metabolism
Contraindications:
- There are very few absolute contraindications to ICS. These include hypersensitivity to the medications and severe hypersensitivity to milk proteins/lactose.
(Liang & Chao, 2021; FDA, 2021b)
INHALED COMBINATION MEDICATIONS
An asthma combination inhaler combines two or three medications, which can ease hyperresponsiveness of airways and help prevent an asthma attack. They are used for the long-term control of asthma symptoms.
| Generic Name | Brand Name |
|---|---|
| Formoterol (LABA) and budesonide (ICS) | Symbicort |
| Formoterol (LABA) and mometasone (ICS) | Dulera |
| Salmeterol (LABA) and Fluticasone (ICS) | Advair Diskus Advair HFA |
| Vilanterol (LABA) and Fluticasone (ICS) | Breo Ellipta |
| Vilanterol/ umeclidinium (anticholinergic) and Fluticasone (ICS) | Trelegy |
(AAFA, 2021h; FDA, 2021b; AAAAI, 2021; Schiffman, 2020; Gottwalt & Tadi, 2021; Liang & Chao 2021)
SYSTEMIC CORTICOSTEROIDS
Systemic corticosteroids, whether administered intravenously or orally, are a key treatment for moderate or severe episodes of asthma. For patients whose asthma attacks do not resolve promptly after inhalation of their rescue medicines, systemic corticosteroids will speed the widening of airways and make a near-term recurrence less likely.
In emergency settings, intravenous corticosteroids are used, and sometimes oral systemic steroids are taken in high doses for several days. This is referred to as a steroid burst.
Oral steroids can also be used to control symptoms in people with severe persistent asthma. When used for this purpose, the drug is taken daily at a lower dose than is used during an asthma exacerbation. The smallest possible dose should be given to avoid long-term effects. Some people can control their symptoms with every-other-day dosing.
| Generic Name | Brand Name |
|---|---|
| Oral prednisone | Prednisone Intensol Rayos |
| Oral prednisolone | Orapred ODT Pediapred Prelone Medrol |
| Injectable methylprednisolone | Dep-Medrol Solu-Medrol |
| Oral methylprednisolone | Medrol |
| Injectable triamcinolone | Kenalog Aristospan Triesence |
Side effects with short-term use:
- Weight gain (fat deposits in abdomen, face, nape of neck)
- Fluid retention
- Upset stomach
- Hypertension
- Mood swings
- Memory or behavior problems
- Confusion or delirium
Side effects with long-term use:
- Growth suppression
- Hyperglycemia
- Cataracts
- Glaucoma
- Osteoporosis and fractures
- Thin skin, bruising, and slower healing
- Muscle weakness
- Increased risk for infections
- Adrenal gland hormone suppression
- Severe fatigue
- Loss of appetite
- Nausea
- Muscle weakness
Precautions:
- When taking steroids chronically, they should not be abruptly discontinued. Tapering the drug allows the adrenal glands time to return to normal secretion patterns.
- Any acute infections should be treated and fully resolved before starting oral corticosteroids.
- Avoid use in patients with adrenal insufficiency.
- Use with caution in people with glaucoma/cataracts and osteoporosis.
- Patients may experience withdrawal symptoms, including:
- Weakness
- Fatigue
- Body aches
- Joint pain
- Decreased appetite
- Weight loss
- Nausea
- Vomiting
- Diarrhea
- Abdominal pain
(Lexicomp, 2021; Pichardo, 2020; FDA, 2021b)
Leukotriene Modifiers
Leukotriene modifiers act on cells that produce leukotrienes, which are lipid compounds released from mast cells, eosinophils, and basophils and that are responsible for airway bronchoconstriction, inflammatory cell recruitment, increased vascular permeability, and secretion production. Leukotriene modifiers work in two ways:
- By binding to cysteinyl leukotrienes receptors and blocking their activation and subsequent inflammatory cascade
- By stopping or inhibiting the production of the enzyme 5-lipoxygenase, a precursor to the production of leukotrienes
Leukotriene modifiers can help prevent symptoms for up to 24 hours, are well tolerated, and appear to work best in patients with mild to moderate persistent asthma. They are often used in addition to inhaled corticosteroids to avoid the use of oral corticosteroids and are an alternative, but not preferred, therapy to low- to medium-dose inhaled corticosteroids.
Guidelines suggest a trial of an antileukotriene in patients with severe asthma who are not controlled on high-dose inhaled corticosteroids and long-acting beta-2 agonists.
| Generic Name | Brand Name |
| Leukotriene receptor agonists | |
|---|---|
| Montelukast | Singulair |
| Zafirlukast | Accolate |
| 5-lipoxygenase inhibitor | |
| Zileuton | Zyflo Zyflo CR |
Side effects of montelukast:
- Headache
- Earache
- Sore throat
- Abdominal pain
- Cough
- Dyspepsia
- Increased risk for respiratory infections
Precautions for montelukast:
On rare occasions montelukast has been linked to psychological reactions such as:
- Insomnia
- Anxiety
- Nightmares
- Aggression
- Hallucinations
- Depression
- Suicidal thinking
Contraindications for montelukast:
- Persons with phenylketonuria (PKU) should not take the chewable tablets that contain aspartame (an artificial sweetener that contains phenylalanine).
Side effects for zafirlukast:
- Headache
- Upper respiratory infections
- Nausea
- Vomiting
- Dyspepsia
- Abdominal pain
- Diarrhea
- Malaise
- Rarely, elevation of liver enzymes, acute hepatitis, and hyperbilirubinemia
Contraindications for zafirlukast:
- Not for use in patients with hepatic impairment.
(Choi & Azmat, 2021; FDA, 2021b)
Immunomodulators
Immunomodulators are asthma therapy medications used to help regulate or normalize the immune system.
MONOCLONAL ANTIBODY THERAPY
Monoclonal antibody (biologic) therapy uses laboratory-produced substitute antibodies to bind to certain cells or proteins. They are add-on maintenance treatments for relief of acute asthma, providing an alternative to systemic corticosteroids.
Omalizumab is a newer asthma medication that may be used for persons with persistent moderate to severe asthma due to seasonal allergies that is not controlled by inhaled corticosteroids. A disadvantage is that it is very expensive ($12,000 to $15,000 per year). Omalizumab works by binding to human immunoglobulin E (IgE) on the surface of mast cells and basophils, resulting in reduced release of allergy-inciting chemicals.
Mepolizumab is also used for moderate to severe asthma. This agent works by binding to interleukin 5, resulting in decreased eosinophils which contribute to the development of asthma attacks.
Anyone over the age of 12 can be given an omalizumab injection every two to four weeks. For individuals with elevated eosinophils, mepolizumab is given by injection every four weeks.
Dupilumab is used for the treatment of moderate to severe eosinophilic asthma in people ages 12 and older. It reduces asthma exacerbations, enables oral corticosteroid tapering, and improves lung function.
| Generic Name | Brand Name |
|---|---|
| Omalizumab (anti- IgE) injection | Xolair |
| Mepolizumab (anti-IL5) injection | Nucala |
| Benralizumab (anti-IL-5) injection (for ages 12 and older) |
Fasenra |
| Reslizumab (anti-IL5) injection (for ages 18 and older) |
Cinquair |
| Dupilumab | Dupixent |
Side effects:
- Pain or swelling in the area of injection
- Oropharyngeal pain
- Eosinophilia
Precautions:
- Omalizumab has the rare potential to induce anaphylaxis, so it must be administered only in a closely observed clinic.
- The FDA has issued a warning about a slight increased risk for heart and brain blood vessel problems with omalizumab, such as ministrokes, heart attacks, hypertension in the pulmonary arteries, and blood clots.
- Avoid use of live vaccines in patients being treated with dupilumab.
(Wenzel, 2021; Schiffman, 2020; Morris, 2020; FDA, 2021b)
MAST CELL STABILIZERS
A mast cell stabilizer is an inhaled medication that prevents the release of histamine and other inflammatory substances from mast cells in response to an allergic that causes asthma. A mast cell stabilizer is not as potent as ICSs.
The only available mast cell stabilizer available for use in asthma is cromolyn sodium solution delivered via nebulizer. It may be used alone or with other asthma medications, such as bronchodilators or corticosteroids.
Symptoms may improve soon after starting cromolyn, but it could take up to 4 weeks before the full benefit of the medication is realized. Frequent dosing is necessary, as its effects last only 6 to 8 hours.
Common side effects:
- Coughing
- Nausea
- Throat dryness or irritation
Rare side effects:
- Dysphagia
- Pruritis
- Increased wheezing
- Dyspnea
- Hypotension
- Swelling of face, lips, or eyelids
- Chest tightness
Contraindications:
- Do not use in children younger than 2 years of age.
Precautions:
- Use with caution in those with heart disease or cardiac arrhythmias.
(Mayo Clinic, 2021b; FDA, 2021b)
Pharmacology Step Therapy
The step treatment of asthma is based on severity of symptoms and the patient’s age. Asthma medications are added or deleted according to the frequency and severity of the patient’s symptoms.
| Step | Asthma Severity | Preferred Therapy |
| (Fanta, 2020b; NHLBI, 2020b) | ||
| Ages 12 Years and Older | ||
|---|---|---|
| 1 | Intermittent |
|
| 2 | Mild persistent |
|
| 3 | Moderate persistent |
|
| 4 | Severe persistent |
|
| 5 | Severe persistent |
|
| Ages 5–11 Years | ||
| 1 | Intermittent |
|
| 2 | Mild persistent |
|
| 3 | Moderate |
|
| 4 | Severe persistent |
|
| 5 | Severe persistent |
|
| 6 | Severe persistent |
|
| Ages 0–4 Years | ||
| 1 | Recurrent wheezing |
|
| 2 | Mild persistent |
|
| 3 | Moderate persistent |
|
| 4 | Severe persistent |
|
| 5 | Severe persistent |
|
| 6 | Severe persistent |
|
For patients whose asthma has been well-controlled for three to six months on a stable regimen, controller medications can be reduced in a step-wise fashion. The purpose for stepping down therapy is to reduce long-term exposure to high doses of inhaled glucocorticoids (Fanta, 2020b).
WHEN TO REFER
Referral to a pulmonologist or allergist/immunologist is recommended in the following circumstances:
- Difficulty confirming a diagnosis of asthma
- A patient has experienced a life-threatening asthma attack
- The patient has required hospitalized or more than two bursts of oral glucocorticoids in a year or inability to discontinue oral glucocorticoids
- Need for step 4 care in adult or child older than 5 years
- Need for step 2 care or higher in a child under 5 years
- Poor asthma control after 3 to 6 months of active therapy and monitoring
- Anaphylaxis or confirmed food allergy
- Presence of complicating comorbidity
- Need for additional diagnostic tests
- Candidate for monoclonal antibody therapy
- Candidate for allergen immunotherapy
- Patients with possible occupational triggers
- Patients with psychosocial or psychiatric problems which interfere with asthma management
(Fanta, 2020b)
Nonpharmacologic Asthma Procedure
For patients with severe asthma that remains unimproved with the use of inhaled corticosteroids or long-term asthma medication, a minimally invasive procedure has been developed known as bronchial thermoplasty.
Bronchial thermoplasty takes place over three hour-long sessions and involves heating the inside of the airways in the lungs with an electrode. This causes a reduction in smooth muscle, which limits the ability of the airways to tighten, thus making it easier to breathe and possibly reducing asthma attacks. Currently, however, this treatment is limited to academic medical centers, which many patients are unable to access (Fanta, 2020b).