ASTHMA INPATIENT MANAGEMENT
When patients are admitted to the hospital following an acute asthma exacerbation, a multidisciplinary team will manage their care, including medicine, nursing, and respiratory therapy.
The purpose for hospitalization is to closely monitor the patient and to have aggressive interventions available in the event the asthma worsens. Hospitalization serves the purpose of removing the patient from the stimuli in the home environment that may have aggravated asthma, to ensure medication compliance, and to permit inactivity during recovery. In many instances, airway obstruction remains unstable, with wide swings in expiratory flow over minutes or hours.
Patients usually will have received bronchodilator treatments, systemic corticosteroids, other medications, and oxygen in the emergency department. Inpatient treatment is often a continuation of those therapies and monitoring progress.
Inpatient Medical Management
Medication and treatment modalities will be ordered by the admitting provider, who determines initial pharmacologic treatment depending on the severity of the patient’s exacerbation. During the patient’s inpatient stay, medical management includes:
MONITORING
- Obtaining ABGs on admission
- Monitoring and responding to changes in vital signs:
- Done on admission and every 4 hours for 12 hours
- After 12 hours, every 6 hours
- Monitoring PEF rate:
- If the patient is on hourly nebulizer treatments, peak flow every hour
- Pre- and post- twice-daily nebulizer treatments
- Monitoring oxygen saturation with spirometry:
- Provide supplemental oxygen to keep O2 saturation adequate (>90% for adults, >95% for children)
- Discontinue when O2 saturation is adequate for 4 hours and patient is on general ward
- Continue spot checks of O2 saturation with vital signs or as needed for respiratory distress
- Telemetry monitoring indications:
- Patient is receiving SABA nebulizer treatments more often than every 4 hours
For infants or young children, corroborate O2 saturation monitor with pulse rate as a child’s movements make oxygen saturation inaccurate. A decrease in oxygen saturation increases pulse rate.
MEDICATIONS
- Administer SABA by nebulizer
- IV methylprednisolone (Solu-Medrol)
- Change to oral prednisone when SABA is spaced at 4 hours or more and patient is tolerating oral intake
EVALUATION
- Arterial blood gases
- Pulmonary function tests. Criteria:
- PEF <30%
- Prior history of pCO2 >40
- Failure to improve in 4 hours of therapy
- Clinical asthma score >7
- Indications to monitor serum electrolytes:
- Nausea or vomiting
- IV fluids administered for >24 hours
- Beta agonist use more often than every 4 hours for 24 hours
- Chest X-ray indications:
- First episode wheezing
- Marked breath sound asymmetry
- History of exam suggestive of pneumonia
- Signs of improvement:
- Minimal or no wheezing
- Less than two awakenings at night due to mild asthma symptoms
- Good activity tolerance
- Pulmonary function test: PEF or FEV1 >70% of baseline
- Adequate O2 saturation off supplemental oxygen
MORE INTENSIVE TREATMENT OPTION
- Admit to intensive care unit if no improvement in 6 to 12 hours
PREPARATION FOR DISCHARGE
- Assess for asthma-related death risk factors:
- Requires inhaled SABA no more frequently than once every 4 hours
- Parenteral steroids switched to oral corticosteroids
- Adequate O2 saturation on room air
- Asthma education, including:
- Instructions and return demonstration for use of inhaled controller medications
- Instruction in obtaining peak flow measurements at home
- Completing a personalized asthma action plan
- Appointment made for follow-up in 7–10 days after discharge
(Moses, 2021)
Inpatient Nursing Management
Upon arrival to a nursing unit, the admitting nurse performs a complete nursing assessment and develops a plan of care that addresses issues according to the patient’s individual needs. In the creation of a care plan, specific problems are identified, related factors are acknowledged, defining characteristics are considered, and a nursing diagnosis is made. Common problems for a patient with asthma may include, but are not limited to:
- Inability to clear airways effectively
- Altered breathing patterns
- Altered exchange of gases in the lungs
- Anxiety
For each nursing diagnosis, short- and long-range measurable and achievable goals are set, followed by nursing interventions that will assist the patient to meet those goals. The plan is implemented, and each intervention and outcome are assessed for effectiveness.
INABILITY TO CLEAR AIRWAYS EFFECTIVELY
Ineffective airway clearance is related to bronchoconstriction, increased mucus production, decreased ciliary action, ineffective cough, and decreased energy or fatigue as evidenced by:
- Abnormal breath sounds
- Abnormal respiratory rate, rhythm, and depth
- Excessive secretions
- Dyspnea
- Hypoxemia/cyanosis
- Inability to cough up secretions
- Ineffective or absent cough
- Orthopnea
Goals/Outcomes
- Patient will maintain clear and open airways as evidenced by:
- Normal breath sounds
- Normal rate/depth of respirations
- Effective cough after treatment and deep breathing
- Increased air exchange
- Patient will explain methods to enhance secretion removal
- Patient will recognize the significant of changes in sputum, including:
- Color
- Character
- Amount
- Odor
- Patient will identify and avoid specific factors that inhibit effective airway clearance
Nursing Assessment
- Airway patency and abnormal breath sounds:
- Decreased or absent breath sounds
- Wheezing (high-pitched whistling)
- Expiratory grunt
- Rales (clicking, rattling, coarse crackles)
- Rhonchi (low-pitched rattle)
- Stridor (high-pitched musical sound)
- Respirations:
- Rate and depth
- Pattern
- Flaring of nostrils
- Dyspnea on exertion
- Evidence of splinting
- Use of accessory muscles
- Position taken for breathing
- Changes in mental status:
- Increased lethargy
- Confusion
- Restlessness
- Irritability
- Vital signs (elevated temperature may indicate infection)
- Effectiveness of cough and productivity
- Sputum
- Quality, amount, color, and consistency
- Signs of infection (odor and discoloration)
- Signs of dehydration (thick, tenacious)
- Submit a sputum specimen for culture and sensitivity testing, as appropriate
- Oxygen saturation, using pulse oximetry
- Arterial blood gases
- Hydration status:
- Skin turgor
- Mucous membranes
- Tongue
- Abdominal or thoracic pain (as possible cause for shallow breathing and ineffective cough)
- Peak airway pressures and airway resistance, if on mechanical ventilation
- Patient’s understanding of the disease process (depending on patient’s acute state as well as cognitive level)
- Patient’s use of herbal treatments that may result in drug interactions with prescribed medications (e.g., echinacea, goldenseal, ma huang)
Nursing Interventions
- Teach and assist with effective ways to remove secretions, i.e., taking a deep breath, holding it for 2 seconds, and then coughing two or three times in succession.
- Position patient in high Fowler’s, if tolerated, to improve lung exchange and air exchange.
- Provide education that includes:
- Proper sitting position to promote use of abdominal muscles for more forceful cough
- Use of pillow or hands to splint the abdomen when coughing
- Use of quad and huff techniques:
- Hold breath for two or three seconds
- Exhale forcefully but slowly to move mucus from smaller to larger airways
- Repeat two more times
- End with one strong cough to clear mucus from larger airways
- Use of incentive spirometry
- Importance of ambulation and frequent position changes
- Proper use of prescribed medications and inhalers
- Need for adequate fluid intake even after discharge
- Perform nasotracheal suctioning PRN, especially if cough is ineffective.
- Maintain humidified oxygen to reduce thickness of secretion.
- Encourage fluid intake to 3 L/day within limits of cardiac reserve and renal function.
- Give medications as prescribed and document effectiveness and side effects.
- Coordinate with respiratory or physical therapy for chest physiotherapy and nebulizer management.
- Provide postural drainage, percussion, and vibration as prescribed.
- Provide oral care every 4 hours.
(Wayne, 2019)
ALTERED BREATHING PATTERN
Breathing pattern alterations can result in inhalations and exhalations do not allow for adequate ventilation. Patients with asthma are prone to dysfunctional breathing patterns most often related to hypoxia, the underlying inflammatory process, tracheobronchial constriction, decreased energy, fatigue, or anxiety as evidenced by:
- Cough
- Cyanosis
- Dyspnea
- Nasal flaring
- Prolonged expiration
- Changes in respiratory depth
- Tachypnea
- Accessory muscle use
Goals/Outcomes
- Reach and maintain optimal breathing pattern as evidenced by:
- Relaxed and normal breathing pattern
- Normal breathing rate
- Absence of dyspnea
Nursing Assessment
- Vital signs for evidence of hypoxia and hypercapnia:
- Decreased blood pressure
- Decreased heart rate
- Respiratory rate, depth, and rhythm for signs of impending respiratory failure:
- Inability to breath, cyanosis related to hypoxemia
- Increased respiratory rate, confusion related to hypercapnia
- Breath sounds for signs of respiratory failure:
- Decreased wheezing
- Indistinct breath sounds
- Relationship of inspiration to expiration
- Signs of dyspnea:
- Flared nostrils
- Chest retractions
- Accessory muscle use
- Conversational dyspnea (inability to converse without difficulty)
- Fatigue (may lead to respiratory failure)
- Presence of pulsus paradoxus greater than 12 mmHg during inspiration (decrease in systolic blood pressure and pulse amplitude during inspiration)
Nursing Interventions
- Plan for periods of rest between activities to reduce metabolic rate and oxygen requirements.
- Maintain elevated head of bed to 45 degrees.
- Demonstrate and encourage diaphragmatic and pursed-lip breathing.
- Administer medications as ordered.
- Monitor oxygen saturation levels (normal is 95%–100%).
- Monitor PEF and FEV1 as taken by respiratory therapy.
(Martin, 2020)
ALTERED EXCHANGE OF GASES IN THE LUNGS
Alterations in the exchange of gases in the lungs results in an excess or deficiency in oxygenation and/or carbon dioxide related to altered oxygen supply due to bronchospasm, mucosal edema, and mucus plug formation as evidenced by the same manifestations as patients with both impaired airway clearance and impaired breathing pattern but also:
- Changes in vital signs above baseline
- Oxygen saturation <90%
- Anxious appearance
- Diaphoresis
- Restlessness
- Irritability
- Confusion
- Altered skin color: pallor, cyanosis, duskiness
- Abnormal lung sounds, rate, rhythm, and depth
- Tripod position
- Dyspnea
Goals/Outcomes
- Absence of respiratory distress signs and symptoms
- Vital signs within patient’s normal limits
- Clear breath sounds
- Oxygen saturation persisting at >90%
- Normal mentation
Nursing Assessment
- Characteristics of respirations (rate, rhythm, depth, use of accessory muscles)
- Oxygen saturation, monitoring continuously
- ABGs, monitoring frequently
- Lung sounds, auscultating at least every 2–4 hours, listening for adventitious breath sounds
- Ability to cough and clear secretions, noting characteristics of sputum: amount, color and consistency
- Skin and mucous membranes, monitoring for peripheral cyanosis (nailbeds) or central cyanosis (lips/earlobes, tongue) (duskiness and central cyanosis indicate advanced hypoxemia)
- Mentation, for irritability, restlessness, and confusion, and lethargy and somnolence as late signs of hypoxia
- Patient’s level of stress and anxiety
- Nutritional status
- Low hemoglobin level
Nursing Interventions
- Monitor oxygen saturation utilizing continuous pulse oximetry.
- Administered oxygen as ordered to maintain oxygen saturation above 90%.
- Administer medications as ordered and assess for effectiveness and side effects.
- Elevate the head of the bed (30 to 45 degrees) to minimize difficulty breathing and promote maximum lung expansion, using high Fowler’s position or over-the-table positioning whenever possible.
- Adjust position frequently to maintain correct body alignment for easier ventilation and gas exchange.
- Encourage prone position as tolerated to increase PaO2.
- Consider a rotorone bed or mattress with a percussion function to help loosen and remove secretions.
- Encourage frequent pulmonary hygiene measures:
- Cough and deep breathing exercises
- Use of incentive spirometry
- As directed by respiratory therapy, use of a flutter valve to loosen secretions (a handheld device that causes airway vibration and positive expiratory pressure)
- Provide small frequent meals and add supplements.
- Encourage ambulation as tolerated.
- Provide rest periods between activities of daily living (ADLs) and pace activities.
- Provide reassurance for the patient who is anxious.
For the critical care patient:
- Anticipate need for intubation
- Suction airway as needed
ANXIETY
Asthma causes stress, which in turn causes anxiety. As symptoms worsen, the patient may become more anxious, which then increases asthma symptoms, resulting in a sensation of panic. Anxiety and stress are also known triggers for asthma exacerbations.
Common factors may include:
- Change in environment
- Change in health status
- Loss of control
- Hypoxia
- Respiratory distress
Common assessment cues include:
- Apprehensiveness
- Dyspnea
- Fear of being left alone in a room
- Restlessness
- Tachycardia
- Tachypnea
Goals/Outcomes
- Use an effective coping mechanism
- Verbalize a reduction in level of anxiety experienced
- Demonstrate reduced anxiety as evidenced by a calm demeanor and cooperative behavior
Nursing Assessment
- Signs of anxiety:
- Feelings of panic, fear, uneasiness
- Tachycardia
- Cold or sweaty hands or feet
- Shortness of breath
- Restlessness
- Oxygen saturation
Nursing Interventions
- Encourage verbalization of concerns.
- Provide comfort measures (e.g., a calm, quiet environment; soft music).
- Explain every procedure in a simple and concise manner.
- Update significant others of the patient’s progress (since family anxiety can be easily transferred to the patient).
- Stay with the patient and encourage slow, deep breathing.
- Assure the patient and significant others of close, consistent monitoring that will ensure prompt intervention.
- Encourage use of relaxation techniques:
- Progressive muscle relaxation
- Diaphragmatic and pursed-lip breathing
- Use of imagery, repetitive phrases
(Martin, 2020)
ASTHMA PATIENT TEACHING
The nursing team has a large role to play in teaching patients and families throughout the inpatient stay, providing education on the asthma disease process and symptom recognition, among other topics. Patient teaching includes:
- Cough and deep breathing methods
- Types of oxygen therapy to be used at home, if applicable
- Early signs of decreased oxygenation and interventions
- Education on smoking cessation and resources that can help
- Correct use of medications:
- Indications for use
- Dosage
- Frequency
- Differentiating between rescue and controller medications and effects
- Demonstration and verification of correct inhaler use
- Demonstration and verification of correct nebulizer use
- Development or updating of the asthma action plan
- Environmental control of triggers and aggravators
- Demonstration and verification of correct peak flow meter use
- Importance of posthospitalization follow-up with the primary care provider
- Consult with occupational therapy to provide education on energy conserving techniques
(RTZ, 2021)
Asthma Inpatient Respiratory Therapy
Respiratory therapists follow and assess patients throughout their hospital stay, adjusting their treatment and educating them according to guidelines. Respiratory therapists:
- Recommend, administer, and evaluate the pharmacology regimen for a patient
- Perform airway clearance:
- Pulmonary hygiene techniques
- Deep breathing exercise
- Chest physiotherapy
- Recommend, administer, and evaluate oxygen therapy
- Perform rest and exercise oximetry
- Perform arterial blood gas sampling and interpretation
- Recommend, administer, and evaluate humidification/aerosol therapy
- Recommend, administer, and evaluate noninvasive positive pressure ventilation therapy
- Recommend, administer, and evaluate airway management
- Recognize the causes of ventilator/respiratory failure and recommend, perform, and evaluate ventilator management
- Establish and maintain mechanical ventilation with a given ventilator
- Perform and interpret pulmonary function tests
(NSCC, 2020)
CHEST PHYSIOTHERAPY
Chest physiotherapy is routinely carried out by both respiratory and physical therapists depending on a facility’s policies and staffing. Chest PT involves a group of treatments meant to eliminate secretions in the airway and works best if applied along with a bronchodilator. The purpose of these treatments is to:
- Facilitate removal of retained airway secretions
- Optimize lung compliance and prevent collapse
- Decrease the work of breathing
- Optimize ventilation-perfusion ratio and improve gas exchange
Postural drainage involves placing the patient in a position in which gravity can assist in airway clearing. Positions vary based on specific segments of the lungs with a large amount of secretions. Each position should generally be held for 3–15 minutes.
Percussion is also called cupping. Its purpose is to intermittently apply kinetic energy to the chest wall and lungs by rhythmically striking the chest with a cupped hand or mechanical device directly over the area of the lung being drained.
Vibration involves the use of a fine tremorous action over the area being drained. The rapid vibratory impulse is transmitted through the chest wall from the hands of the therapist to loosen and dislodge the airway secretions (Physiopedia, 2021b).
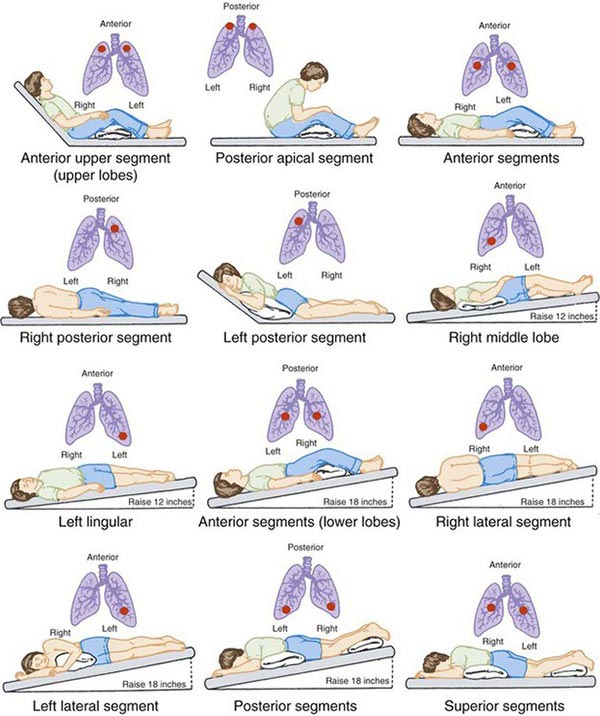
Postural drainage positions. (Source: Adapted from Potter & Perry, 1997.)
(See also “Physical Therapy Management” later in this course.)