COMMON MEDICAL ERRORS AND HOW TO PREVENT THEM
Medical errors are likely to occur in situations where providers are challenged to make decisions in dynamic, fast-paced, complex environments under tight time constraints. Errors stem from technical, organizational, or human factors that set off a chain reaction that could result in an adverse event (Carver et al., 2020).
The ten most common causes of medical error include:
- Altered ability to make good judgments and quick decisions (e.g., misapplying expertise)
- Ineffective communication (the most common cause)
- Deficiencies in education, training, orientation, and experience
- Inadequate methods of identifying patients, incomplete assessment on admission, failing to obtain consent, and failing to provide education to patients
- Inadequate policies to guide healthcare workers
- Lack of consistency in procedures
- Inadequate staffing and/or poor supervision
- Technical failures associated with medical equipment
- No audits in the system
- No one prepared to accept responsibility or change the system
(Rodziewicz et al., 2021)
Surgical Errors
Wrong-site, wrong-procedure, and wrong-patient surgical errors are relatively rare. It is estimated that in the United States such errors occur in approximately 1 of 112,000 surgical procedures and are infrequent enough that an individual hospital would only experience one such incident every 5 to 10 years. However, this includes only procedures performed in an operating room. If procedures performed in other settings such as ambulatory surgery are included, the rate of error may be much higher (AHRQ, 2019d).
Retained foreign bodies (also called retained surgical items) and unintentionally retained foreign objects are defined as objects retained after skin closure following an invasive procedure. Most unintended retained foreign bodies are associated with failures in leadership, communication, or other human factors that should be under the control of the operating team (Pellegrini, 2019).
Anesthesia-related adverse events may include inadvertent gas flow change, premature extubation, or breathing circuit connection error (Rayan et al., 2019).
PREVENTING SURGICAL ERRORS
The WHO Surgical Safety Checklist was developed after extensive consultation aimed at decreasing errors and adverse events, and increasing teamwork and communication in surgery. This checklist has gone on to show significant reduction in both morbidity and mortality and is now used by a majority of surgical providers around the world (WHO, 2021).
ELEMENTS OF THE WHO SURGICAL SAFETY CHECKLIST
A surgical checklist is an algorithmic listing of actions to be taken in any given clinical situation intended to make everyone aware that others expect these things to be done.
“SIGN IN” checklist must be completed orally and in writing before induction of anesthesia (with at least a nurse and anesthetist).
- Has the patient confirmed their identify, site, procedure, and consent?
- Is the site marked?
- Is the anesthesia machine and medication check complete?
- Is the pulse oximeter on the patient and functioning?
- Does the patient have a:
- Known allergy?
- Difficult airway or aspiration risk?
- Risk of >500 ml blood loss (7 ml/kg in children)?
“TIME OUT” checklist must be completed orally and in writing before skin incision (with nurse, anesthetist, and surgeon).
- Confirm all team members have introduced themselves by name and role
- Confirm the patient’s name, procedure, and where the incision will be made
- Has antibiotic prophylaxis been given within the last 60 minutes?
- For the anticipated critical event:
- To surgeon:
- What are the critical or nonroutine steps?
- How long will the case take?
- What is the anticipated blood loss?
- To anesthetist:
- Are there any patient-specific concerns?
- To nursing team:
- Has sterility (including indicator results) been confirmed?
- Are there equipment issues or any concerns?
- To surgeon:
- Is essential imaging displayed?
“SIGN OUT” checklist must be completed orally and in writing before the patient leaves the operating room (with nurse, anesthesia provider, and surgeon).
- Nurse verbally confirms:
- The name of the procedure
- Completion of instrument, sponge, and needle counts
- Specimen labeling (read aloud specimen labels, including patient name)
- Whether there are any equipment problems to be addressed
- To surgeon, anesthetist, and nurse:
- What are the key concerns for recovery and management of this patient?
(WHO, 2021)
Medication Errors
Every year in the United States, 7,000 to 9,000 people die due to a medication error. In addition, hundreds of thousands experience but often do not report an adverse reaction or other complication related to a medication (Tariq et al., 2021).
Medication errors may be due to human errors but often result from a flawed system with inadequate backup to detect mistakes. Medication errors may occur at any step, including:
- Ordering/prescribing. The clinician must select the appropriate medication, dose, frequency, and duration.
- Transcribing. In a paper-based system, an intermediary must read and interpret the prescription correctly.
- Dispensing. The pharmacist must check for drug-drug interactions and allergies and release the appropriate quantity of the medication in the correct form.
- Administering. The correct medication must be supplied to the correct patient at the correct time, either by a nurse, other trained staff, patient, or caregiver.
- Monitoring. This includes laboratory tests, side effects, effectiveness of therapeutic action, and vital signs.
- Documenting. The name, strength, and quantity of drug; the date and time administered; and the name of the person administering the drug must be entered in the patient’s medication administration record in a timely manner.
(Tariq et al., 2021)
PREVENTING ERRORS IN PRESCRIBING AND TRANSCRIBING
Errors occur most commonly during the ordering/prescribing and transcribing stages, accounting for almost 50% of medication errors. Even with the increasing use of electronic health records, which has helped avert errors at the ordering and transcribing stages, such errors continue to occur.
The first line of defense against medication errors should be the prescribing clinician, who must have all the information needed to make the best possible prescribing decisions for each patient. Strategies for preventing errors when prescribing include avoiding unnecessary medications by adhering to conservative prescribing principles, which include:
- Maintaining heightened awareness concerning side effects
- Exercising skepticism about new drugs
- Remaining alert for high-risk medications
- Involving the patient in decision-making
- Considering long-term impacts of medications prescribed
- Considering patient age and body weight
- Considering liver and kidney function
Use of a computerized provider order entry (CPOE) avoids the necessity for transcribing an order and thus reducing risk of error.
Medication reconciliation (reviewing each medication and comparing it against the medication administration record) can be performed at times of transitions in care between facility units or another facility, or upon discharge to home.
To reduce transcription errors, a double-check procedure is recommended in which another nurse on the same shift or incoming shift reviews all new orders to ascertain that each order is correctly noted and transcribed on the physician’s order and on the medication administration record. Read-back to another professional is another procedure in which a nurse reads back an order to the prescribing physician or another nurse to make certain the medication ordered is correctly transcribed (APF, 2020; Saljoughian, 2020).
“DO NOT USE” ABBREVIATION LIST
Misreading medical abbreviations can be a cause of serious medication errors, and the Joint Commission has created a “do not use” list of abbreviations that endanger patients’ safety and that it requires its members to follow.
| Do Not Use | Potential Problem | Instead Use |
|---|---|---|
| (TJC, 2020) | ||
| U, u | Mistaken for “0” (zero), the number “4” (four), or “cc” | Unit |
| IU | Mistaken for IV (intravenous) or the number 10 (ten) | International unit |
| Q.D., QD, q.d., qd | Mistaken for each other | Daily |
| Q.O.D., QOD, q.o.d, qod | Period after the “Q” mistaken for “I” and the “O” mistaken for “I” | Every other day |
| Lack of leading zero | Decimal point is missed | 0.X mg |
| MS | Can mean morphine sulfate or magnesium sulfate | Morphine sulfate or Magnesium sulfate |
| MSO4 and MgSO4 | Confused for one another | Magnesium sulfate |
| Trailing zero * | Decimal point is missed | X mg |
| * Exception: A “trailing zero” may be used only where required to demonstrate the level of precision of the value being reported, such as for laboratory results, imaging studies that report size of lesions, or catheter/tube sizes. It may not be used in medication orders or other medication-related documentation. | ||
PREVENTING ERRORS IN DISPENSING
Dispensing medications involves preparing and packaging a prescription drug or device in a container and labeling the container with information required by state and federal law.
Dispensing errors in U.S. clinical and community pharmacies occur at an average rate of 4 in 250 prescriptions. Forty-one percent of all medication incidents related to information technology are due to choosing the wrong drug. One third of incidents are associated with confusion of similar drug names, and nearly half were associated with drug strength confusion. The most common causes for dispensing errors involve:
- Workload
- Similar drug names
- Interruptions
- Lack of support staff
- Insufficient time to counsel patients
- Illegible handwriting
(Tariq et al., 2021)
Strategies to reduce the risk of medication dispensing errors include:
- Verifying the prescription entry is correct
- Clarifying any ambiguous information such as prescriptions that are illegible or use nonstandard abbreviations and other symbols
- Checking prescriptions thoroughly and verifying by another person
- Providing patient counseling
- Checking for drug-to-drug interactions and allergies
- Supervising dispensing medications by pharmacist assistants
- Opening containers and showing them to the patient (patients may raise an alert if the medication looks different from what they usually take)
- Using tall-man lettering (TML), a technique that uses uppercase lettering to highlight the differences between similar drug names by capitalizing dissimilar letters (e.g., “CISplatin” vs. “CARBOplatin”)
- Using barcode scanners to check whether the selected drug from the shelf is the same as the selected drug on the dispensing screen
(Campmans et al., 2018; FDA, 2020)
PREVENTING ERRORS IN ADMINISTRATION
In the administration stage, errors include:
- Failing to follow the “five rights” to medication administration:
- Right patient
- Right drug
- Right dose
- Right route
- Right time
- Failing to educate the patient as to why the drug is being prescribed
- Leaving a medication at the bedside without knowing if it was taken
- Omitting medications
- Administering an unauthorized medication
- Not shaking a medication that should be shaken before use, leading to overdose or underdose
- Crushing medications not intended to be crushed
- Failing to follow facility policies and procedures
(Hanson & Haddad, 2020)
In inpatient settings, interventions to prevent medication administration errors include:
- Barcoding for both medications and patients
- Adherence to the “five rights” of medication safety
- Smart infusion pumps for intravenous administration
- Single-use medication packages
- Package design features such as tall-man lettering for look-alike drug names
- Minimizing interruptions
Few of these interventions are likely to be successful in isolation, and efforts to improve safe medication use must also focus on transitions to home, primary care, and patient caregiver understanding and administration of medication. These efforts include:
- Patient education
- Revised medication labels to improve patient comprehension of administration instructions
- Multicompartment medication devices for patients taking multiple medications in ambulatory or long-term care settings
(AHRQ, 2019d)
PREVENTING ERRORS IN MEDICATION MONITORING
Monitoring and assessment are essential to the process of administration of medications. Monitoring involves observing the patient to determine if the medication is working, is being used appropriately, and is not harming the patient. Types of errors in monitoring that can occur include:
- Failure to monitor effectiveness of therapeutic action of a medication
- Lack of awareness of side effects of a medication
- Failure to monitor, assess, and report laboratory tests
- Failure to monitor, assess, and report vital signs
- Failure to educate patients about potential side effects
- Failure to comply with a pain management program
- Communication failures during handoff procedures to accepting nurse
(Tariq et al., 2021; AHRQ, 2019d)
PREVENTING ERRORS WITH HIGH-ALERT MEDICATIONS
High-alert medications are drugs that have a heightened risk for causing significant harm when used in error. The FDA requires such drugs be given a label referred to as black box warning. The Institute for Safe Medication Practices maintains a current listing of such medications and makes the following recommendations for reducing error:
- Standardize the ordering, storage, preparation, and administration of these medications.
- Improve access to information about these drugs.
- Limit access to high-alert medications.
- Use auxiliary labels and automated alerts.
- Employ redundancies—duplicate devices used for backup purposes to prevent or recover from the failure of a specific part of the process (e.g., asking another nurse to perform an independent check)
- In community/ambulatory settings, provide mandatory patient education.
(ISMP, 2018)
Tubing Misconnections
The FDA reports that medical device misconnections can occur when one type of medical device is attached in error to another type of medical device that performs a different function. Tubing misconnections can occur for several reasons, including:
- Similar design of many connectors and the widespread use of connectors with similar shapes and in similar sizes
- Human error arising from conditions such as:
- Multiple connections for one patient
- Poor lighting
- Lack of training
- Time pressure
- Fatigue
- High-stress environment
EXAMPLES OF TUBING MISCONNECTIONS
- Enteral feeding tube connected to an IV
- Enteral feeding tube connected to ventilator-inline suction catheter
- Blood pressure cuff tubing connected to an IV port
- IV tubing connected to trach cuff
- IV tubing connected to nebulizer
- Oxygen tubing connected to a needleless IV port
- IV tubing connected to nasal cannula
- Syringe connected to trach cuff
- Epidural solution connected to a peripheral or central IV catheter
- Epidural line connected to an IV infusion
- Bladder irrigation solution utilizing primary IV tubing connected to a peripheral or central IV catheter
- Foley catheter connected to NG tube
- IV infusion connected to an indwelling urinary catheter
- IV infusion connected to an enteral feeding tube
- Primary IV tube connected to a blood product meant for transfusion
(FDA, 2017)
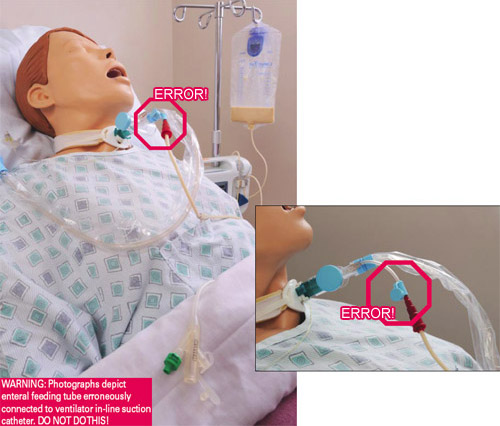
Patient’s feeding tube is incorrectly connected to the instillation port on the ventilator in-line suction catheter, delivering tube feeding into the patient’s lungs, causing death. (Source: FDA, 2017.)
PREVENTING TUBING MISCONNECTIONS
Attempts to prevent device misconnections have included color-coding, labels, tags, and training. However, these methods alone have not effectively solved the problem, because they have not been consistently applied, nor do these methods physically prevent the misconnections.
In order to reduce the chances of tubing misconnections, non-Luer lock connections have been introduced. These include the NR-Fit connector for neuraxial and regional anesthesia catheters and the Enfit connectors for feeding tubes.
These connectors are designed to be incompatible with Luer adaptors, which are commonly used in IV applications. The connectors look and secure very similar to a Luer threaded lock system, although the design is larger and, therefore, incompatible with connectors for unrelated delivery systems such as trach tubes, IV lines, and catheters (Rodziewicz et al., 2021).
Until new connectors are universally adopted, the following interventions offer healthcare providers with strategies such as the use of ACT to prevent device misconnections (see table):
| Label | Step | Actions |
|---|---|---|
| (FDA, 2018) | ||
| A | Assess equipment |
|
| C | Communicate |
|
| T | Trace |
|
Healthcare-Associated Infections (HAIs)
HAIs are infections that occur while receiving healthcare in a hospital or other healthcare facility and that first appear 48 hours or more after admission or within 30 days after having received healthcare. HAIs are considered system failures and are often preventable (CDC, 2020a).
One of the most important reasons in healthcare settings for the spread of bacteria, some of which are antibiotic-resistant and can prove life threatening, is the failure of physicians, nurses, and other caregivers to practice basic hand hygiene. Studies show that on average healthcare providers clean their hands less than half of the times they should, contributing to the spread of HAIs (CDC, 2020b).
PREVENTING CATHETER-ASSOCIATED URINARY TRACT INFECTIONS
Catheter-associated urinary tract infections (CAUTIs) occur at a rate of approximately 3% to 10% per day of catheterization, making duration of catherization an important risk factor. Complications of CAUTIs include sepsis, bacteremia, and involvement of the upper urinary tract (Fekete, 2020).
The CDC (2019a) recommends the following actions supported by evidence-based research for preventing urinary tract infections:
- Insert catheters only for appropriate indications.
- Leave catheters in place only as long as needed.
- Avoid use of urinary catheters in patients and nursing home residents for management of incontinence.
- Avoid routinely using urinary catheters in operative patients unless necessary.
- Perform hand hygiene immediately before and after insertion or any manipulation of catheter device or site.
- Ensure that only properly trained persons insert and maintain catheters.
- In acute care hospital settings, insert catheters using aseptic technique and sterile equipment.
- In nonacute care settings, use clean technique for intermittent catheterization.
- If ultrasound bladder scanners are used, ensure that equipment is cleaned and disinfected between patients.
- Properly secure indwelling catheters after insertion to prevent movement and urethral traction.
- Unless clinically indicated, use the smallest-bore catheter possible consistent with good drainage.
- Follow aseptic insertion and maintain a closed drainage system.
- If breaks in aseptic technique, disconnection, or leakage occur, replace the catheter and collection system.
- Maintain unobstructed urine flow.
- Keep collecting bag below level of bladder at all times.
- Do not rest collecting bag on the floor.
- Empty collecting bag regularly using separate, clean container for each patient; avoid contact of spigot with the container.
- Obtain urine samples aseptically. If small amount needed, aspirate from needleless sampling port with sterile syringe/cannula adapter after cleaning the port with a disinfectant.
- If obstruction occurs and catheter material is contributing to obstruction, change the catheter.
- Comply with CDC hand hygiene recommendations and Standard Precautions.
Also consider:
- Alternatives to indwelling urinary catheterization in selected patients
- Urinary catheter systems with preconnected, sealed catheter-tubing junctions
- Use of portable ultrasound devices for assessing urine volume to reduce unnecessary catheterizations
PREVENTING SURGICAL SITE INFECTIONS
Surgical site infections (SSIs) occur in 2% to 4% of all patients undergoing inpatient surgical procedures. Although most infections are treatable with antibiotics, SSIs remain a significant cause of morbidity and mortality after surgery. They are the leading cause of readmissions to the hospital following surgery, and approximately 3% of patients who contract an SSI will die as a result (AHRQ, 2019e).
The CDC recommends the following measures for the prevention of surgical site infections:
- Administer preoperative antimicrobial agents in accordance with clinical practice standards and guidelines.
- In clean and clean-contaminated procedures, do not administer additional prophylactic antimicrobial agent doses after the surgical incision in closed in the OR, even in the presence of a drain.
- Do not apply antimicrobial agents to the surgical incision with the aim of preventing SSI.
- Consider the use of triclosan-coated sutures for the prevention of SSI.
- Implement perioperative glycemic control in all patients.
- Maintain perioperative normothermia.
- Advise patients to shower or bathe the entire body with either antimicrobial or nonantimicrobial soap or an antiseptic agent the night prior to surgery.
- Perform intraoperative skin preparation with an alcohol-based antiseptic agent unless contraindicated.
- Consider intraoperative irrigation of deep or subcutaneous tissues with aqueous iodophor solution.
- Do not withhold transfusion of necessary blood products from patients undergoing prosthetic joint arthroplasty as a means of preventing SSI.
(Singhal, 2019)
PREVENTING CENTRAL LINE–ASSOCIATED BLOODSTREAM INFECTIONS
Central line–associated bloodstream infections (CLABSIs) are laboratory-confirmed bloodstream infections that are not secondary to an infection at another body site, due to the presence of an intravascular catheter that terminates at or close to the heart, or in one of the great vessels that is used for infusion, withdrawal of blood, or hemodynamic monitoring (NHSN, 2021).
AHRQ (2018) guidelines for prevention of CLABSIs include the following:
Catheter Insertion
- Use aseptic technique:
- Use appropriate hand hygiene using soap and water or a waterless hand sanitizer.
- Use face mask, cap, and sterile gloves.
- Wear a sterile gown with neck snaps and wrap-around ties properly secured.
- Instruct anyone assisting to wear the same barriers.
- Cover the patient entirely with a large sterile drape.
- Create a sterile working surface that acts as a barrier between the insertion site and any possible source of contamination.
- Prepare skin with antiseptic/detergent chlorhexidine 2% in 70% isopropyl alcohol.
- Apply a sterile dressing to the insertion site before the sterile barriers are removed.
- Transparent dressings are preferred to allow visualization of the site.
- Use chlorohexidine for skin preparation.
- Use full barrier precautions during central venous catheter insertion.
- Avoid using the femoral vein for catheter in adult patients.
CV Catheter Site Selection
- Use the subclavian site unless medically contraindicated (anatomic deformity, coagulopathy, renal disease that may require dialysis).
- If the internal jugular vein is chosen, use the right side to reduce risk of noninfectious complications since it has a larger diameter and a straighter path to the superior vena cava.
CV Catheter Selection
- Use a single-lumen central venous access device (CVAD) for patients requiring long-term access (more than 30 days) or a PICC or cuffed CVAD for patient requiring access for greater than 2 weeks.
Arterial Line Site Selection
- Radial artery is the preferred site.
- Dorsalis pedis is the alternative site.
- Femoral sites have higher infection rates, brachial/maxillary site are last resort.
Postinsertion Care
- Evaluate the need for CVAD daily.
- Remove catheter when not needed or change to a single-lumen CVAD when possible.
- Replace the dressing when it becomes damp, loosened, or soiled.
- Replace gauze dressing used on short-term central venous catheter (CVC) sites every 2 days.
PREVENTING PERIPHERAL IV CATHETER–RELATED BLOODSTREAM INFECTIONS
Peripheral vascular catheter (PVC)-associated bloodstream infections occur in approximately 0.18% of patients (Blauw et al., 2019). Guidelines for prevention of peripheral IV catheter-related bloodstream infections include the following:
Site Selection
- In adults, use an upper-extremity site for catheter insertion.
- In pediatric patients, use the upper or lower extremities or the scalp (in neonates or young infants).
Catheter Selection
- Avoid use of steel needles for administration of fluids and medications that might cause tissue necrosis if extravasation occurs.
- Use a midline catheter or peripherally inserted central catheter (PICC), instead of short peripheral catheter, when duration of IV therapy will exceed six days.
Catheter Insertion
- Perform hand hygiene before insertion.
- Prepare clean skin using a chlorhexidine-based solution. If contraindicated, tincture of iodine, an iodophor or 70% alcohol can be used. Allow to dry prior to placing catheter.
- Maintain aseptic technique for insertion of peripheral IV (PIV).
- Wear clean gloves, rather than sterile, for insertion of a peripheral intravenous catheter if the access site is not touched after application of skin antiseptics.
- Use maximal sterile barrier precautions (cap, mask, sterile gown, sterile gloves, and sterile full body drape) for insertion of PICCs.
- Use either sterile gauze or sterile, transparent, semipermeable dressing to cover site.
Catheter and Site Care
- Perform hand hygiene procedures before and after palpating catheter insertion sites as well as before and after, replacing, accessing, repairing, or dressing an intravascular catheter.
- Evaluate catheter insertion site daily both visually and by palpation through the dressing to discern tenderness and by inspection if a transparent dressing is in use. If local tenderness or other signs of possible infection occur, an opaque dressing should be removed and the site inspected visually.
- Replace catheter site dressing if it becomes damp, loosened, or visibly soiled.
- Do not use topical antibiotic ointment or creams on insertion sites, except for dialysis catheter.
- Remove peripheral venous catheter if patient develops signs of phlebitis, infection, or a malfunctioning catheter.
- Wear either clean or sterile gloves when changing the dressing on catheter sites.
- Replace dressing every 7 days for transparent dressing, except in pediatric patients in which risk for dislodging catheter may outweigh the benefit.
- Do not submerge catheter or catheter site in water; cover during showering.
- In both adult and pediatric patients, leave peripheral venous catheters in place until IV therapy is completed, unless a complication occurs.
- For catheters inserted under emergency conditions, insert a new catheter at a different site within 24 hours.
- Encourage patients to report any changes in their catheter site or any new discomfort to their provider.
Replacement of Administration Sets
- Replace administration sets, including secondary sets and add-on devices, no more frequently than at 96-hour intervals, unless clinically indicated.
- Replace tubing used to administer blood, blood products, or lipid emulsions within 24 hours of initiating the infusion.
(Jacob & Gaynes, 2020; CDC, 2017a)
PREVENTING CLOSTRIDIOIDES DIFFICILE INFECTIONS (CDIs)
Clostridioides (Clostridium) difficile (C. diff) infections cause life-threatening diarrhea. It is usually a side-effect of taking antibiotics. Those most at risk are patients, especially older adults, who take antibiotics and people staying in hospitals and nursing homes for a long period of time (CDC, 2019b). Strategies for the prevention of Clostridioides (formerly known as Clostridium) difficile infection include the following:
- Isolate and initiate Contact Precautions for suspected or confirmed CDI.
- Maintain Contact Precautions for at least 48 hours after diarrhea has resolved, or longer, up to the duration of hospitalization.
- Adhere to recommended hand hygiene practices.
- Use dedicated patient-care equipment (e.g., blood pressure cuffs, stethoscopes).
- Implement daily patient bathing or showering with soap and water.
- When transferring patients, notify receiving wards or facilities about the patient’s CDI status.
- Perform daily cleaning of CDI patient rooms using C. difficile sporicidal agent at least once a day, including toilets.
- Clean and disinfect all shared equipment prior to use with another patient (e.g., wheelchair).
- Perform terminal cleaning after CDI patient transfer/discharge using a C. difficile sporicidal agent.
- Clean additional areas that are contaminated during transient visits by patients with suspected or confirmed CDI (e.g., radiology, emergency rooms, physical therapy) with C. difficile sporicidal agent.
- Restrict use of antibiotics with the highest risk for CDI (e.g., fluroquinolones).
- Ensure that patients receive the shortest effective duration of antibiotic therapy.
- Limit use of nonantibiotic patient medications (e.g., proton pump inhibitors, H2-receptor blockers) that are hypothesized to increase risk for CDI.
- Consider additional disinfection of CDI patient room with no-touch technologies (e.g., UV light).
- Dedicate healthcare personnel to care only for patients with CDI only to minimize risk of transmission to others.
(CDC, 2017b)
PREVENTING MULTIDRUG-RESISTANT ORGANISM (MDRO) INFECTIONS
The CDC recommends the use of Contact Precautions in inpatient acute care settings for patients known to be colonized or infected with epidemiologically important MDROs, including methicillin-resistant Staphylococcus aureus (MRSA). However, there is debate as to the most beneficial way to manage patients with MDRO infections.
Based on current evidence, the CDC continues to recommend the use of Contact Precautions for MRSA-colonized or infected patients. The CDC will continue to evaluate the evidence on Contact Precautions as it becomes available.
In acute care hospitals, CDC recommendations state:
- Promote the judicious use of antimicrobial agents.
- Follow Standard Precautions during all patient encounters in all healthcare settings.
- Use a mask according to Standard Precautions when:
- Performing a splash-generating procedure
- Caring for patients with open tracheostomies
- In circumstances where there is evidence of transmission from heavily colonized sources, such as burn wounds
- Not recommended during routine care
- Implement Contact Precautions for all patients known to be colonized/infected with target MDROs.
In long-term care facilities:
- Consider the individual patient’s clinical situation and prevalence or incidence of MDROs in the facility when deciding whether to implement or modify Contact Precautions in addition to Standard Precautions for a patient infected or colonized with a target MDRO.
In ambulatory and home care settings:
- Follow Standard Precautions.
- Limit the amount of reusable patient care equipment that is brought into the home of patients infected or colonized with MDROs.
(CDC, 2020c)
PREVENTING HOSPITAL-ACQUIRED PNEUMONIA LUNG INFECTIONS
Hospital-acquired pneumonia (HAP) occurs 48 hours or more after hospital admission at a rate of 5 to 10 per 1,000 hospital admissions. Ventilator-associated pneumonia (VAP) is a subset of HAP occurring in intensive care units that presents more than 48 to 72 hours after tracheal intubation (Shebl & Gulick, 2020).
Strategies for the prevention of ventilator-associated pneumonias include:
- Use of routine infection control practices and hand hygiene
- Prophylactic antibiotic administration
- Sedation interruption
- Keeping head of bed elevated 30 to 45 degrees
- Limitation of ventilation times
- Endotracheal suctioning
- Avoiding gastric overdistention
- Draining ventilator tube condensate
- Kinetic bed therapy
- Changing ventilator circuit if visibly soiled or mechanically malfunctioning
- Using sterile suctioning techniques and handling of respiratory equipment
- Performing oral care at least every 2 to 4 hours with an antiseptic swab and brushing the teeth twice a day
(Shebl & Gulick, 2020)
Falls
Falls are the most common type of accidents in people 65 years of age and older. Falls in institutional settings occur more frequently and are associated with greater morbidity than falls that occur in the community. Approximately 50% of individuals in the long-term care setting fall yearly (Appeadu & Bordoni, 2020; Kiel, 2020).
Falls risk can be categorized as either intrinsic or extrinsic. Intrinsic factors include issues that are unique to the individual and concern medical, psychological, and physical issues such as advanced age, inner ear disorders, and lower extremity weakness (Appeadu & Bordoni, 2020). Extrinsic factors generally can be changed and address environmental risks that patients encounter, such as use of restraints, dim lighting or glare, ill-fitting or inappropriate footwear (AHRQ, 2017).
Older patients are not the only population at risk. Any patient who has had excessive blood loss may experience postural hypotension, increasing the risk of falling. Maternity patients or other patients who have epidural anesthesia are at risk for falls due to decreased lower-body sensation (AHRQ, 2017b).
PREVENTING FALLS
Preventing falls involves assessing patients for risk for falls, developing a personalized plan of care, and utilizing consistent preventive interventions.
Hospitalized Patients
A fall risk assessment should be done on admission, and reassessment should be done whenever there is a change in a patient’s condition or when a patient is being transferred to another unit. While some institutions have created their own assessment tools, tools that have been extensively studied and recommended include:
- Morse Fall Scale
- STRATIFY Scale
- Schmid Fall Risk Assessment Tool
Some examples of tailored prevention interventions include:
- Physical therapy evaluation/treatment for gait instability
- Toileting schedule for incontinence
- Continuous virtual monitoring for agitation, confusion, or impaired judgment
- Pharmacy consults for medication side effects
(Dykes et al., 2018)
Community-Dwelling Patients
The Centers for Disease Control and Prevention’s STEADI (Stop Elderly Accidents, Deaths and Injuries) initiative is a coordinated approach for the implementation of practice guidelines for fall prevention in community-dwelling adults. It consists of these three core elements:
- Screen for fall risk annually or any time the patient presents with an acute fall
- Assess those who are found to be at risk
- Intervene to reduce identified risk factors
(CDC, 2020d)