IMPACTS AND EPIDEMIOLOGY OF HEART FAILURE
Nurses and other healthcare professionals are charged with giving culturally competent healthcare that recognizes the following epidemiologic factors.
Occurrence
Heart failure affects more than 26 million people globally. It is considered a global epidemic, particularly in countries with rapidly aging populations, such as the United States and Japan. In countries where successful treatment of cardiovascular disease has improved life expectancy in general, the aging population also causes an increase in the occurrence of HF (Salam et al., 2020). HF prevalence is lowest in west sub-Saharan Africa (0.74 per 1000 in males and 0.57 per 1000 in females) (Benjamin et al., 2020).
HF affects approximately 6.9 million people in the United States and is projected to rise to more than 8 million by 2030. Approximately 650,000 people are newly diagnosed with HF each year (Virani et al., 2020; CDC, 2020a; Urbich et al., 2020).
This is attributed to three confounding factors in the population:
- People are living longer, and the elderly population is rapidly increasing, with more people in their 80s and 90s surviving with HF.
- People with acute coronary syndrome are surviving for much longer after an insult such as myocardial infarction due to earlier recognition of coronary artery disease, use of beta receptor blocking agents, and early intervention to improve coronary artery blood flow and preserve ejection fraction.
- The incidence of obesity and diabetes is increasing related to diet and exercise and affecting younger patients ages 20 to 45, who are experiencing heart failure in unprecedented numbers.
(Benjamin et al., 2020)
Heart failure is the most common reason for hospital admissions in adults over 65 years old in the United States. Most HF hospitalizations are caused by one of five precipitants: infection, ischemia, dysrhythmia, medications, and noncompliance with diet. Patients hospitalized with worsening HF are at high risk of rehospitalization. Among patients with a single identifiable precipitant, research shows that the one-year risk for HF readmission varies with the particular precipitant. The precipitant for HF rehospitalizations is more likely to be the same precipitant as for the initial admission (Wang et al., 2020).
Cost
The annual cost of HF is over $6.5 trillion globally. The annual cost of HF in the United States is over $30.7 billion dollars, with over half of that amount spent on hospitalizations. Other expenses include healthcare services, medications to treat heart failure, and days lost from work. With the aging of the population, the total annual cost of HF in the United States is projected to reach $69.8 billion by 2030 when hospitalization, physician, pharmaceutical, and home healthcare costs are all considered (Benjamin et al., 2020; CDC, 2020a).
The annual median medical costs for heart failure care in the United States are estimated at $24,383 per patient. The costs are driven by heart failure–specific hospitalizations, with the median hospitalization cost per admission estimated at $15,879 per patient (Urbic et al., 2020).
Heart failure is the second most commonly diagnosed inpatient condition billed to Medicare. Patients with HF who are admitted to an acute care hospital are medically vulnerable and have a poor prognosis, with a 2-year readmission-free survival rate as low as 17%. Risks for death and rehospitalization immediately after inpatient discharge for HF patients are greatly increased, with much of the economic burden resulting from costly hospital readmissions (Blum et al., 2020).
Mortality
In 2018, heart failure appeared on 379,800 death certificates in the United States as the primary cause of death and accounted for 13.4% of all deaths. Geographically, the preponderance of deaths due to HF are in the southern and midwestern states (CDC, 2020a).
Despite improved technology and medications for treating HF, the mortality rate for HF patients who must be admitted or readmitted to an acute care hospital remains high. A longitudinal study of 73,802 HF patients found that 13.3% died within 30 days of discharge and that the total number of 30-day unplanned readmissions was 6.8% (Roshanghalb et al., 2020).
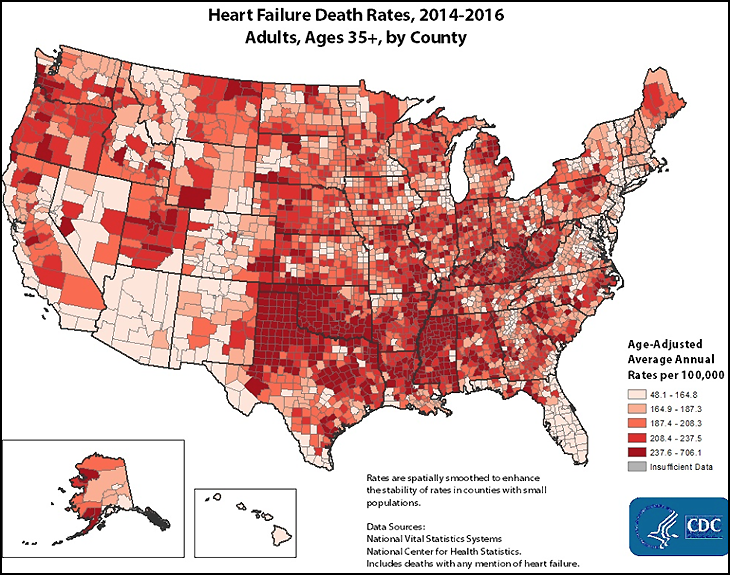
(Source: CDC, 2020a.)
By Age
The incidence of HF in the United States after the age of 65 is 2.1%. Improved survival rates in this population are due to improved technology and medications, and this has resulted in an older group of surviving, chronic HF patients (Benjamin et al., 2020).
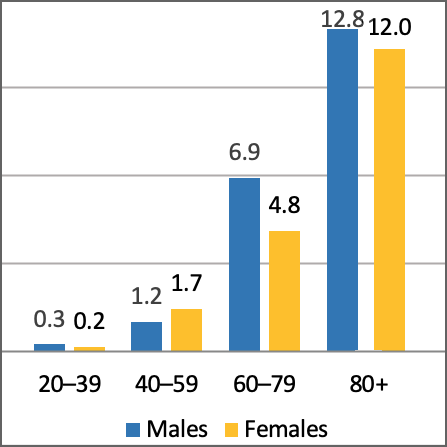
Percent of population with heart failure among U.S. adults by sex and age, 2013–2016. (Source: National Health and Nutrition Examination Survey, 2013–2016.)
Racial and Ethnic Disparities
African Americans have a higher incidence of heart failure, develop symptoms at an earlier age, and experience mortality at a younger age than Whites with the same disease. African Americans with HF who are 65 years and older have more frequent hospitalizations and a mortality rate 2.5 times higher than Whites. This may be explained by African Americans’ higher incidence of comorbid hypertension and diabetes than Whites. Disparities in access to healthcare may also contribute to their earlier morbidity and mortality.
African Americans are usually diagnosed with HF at an earlier age but show greater improvement with compliance with treatment. African Americans have the highest risk of developing HF, followed by Latinx, White, and Chinese Americans, in that order. This higher risk in African Americans reflects differences in the prevalence of hypertension, diabetes, and low socioeconomic status.
African Americans had the highest proportion of incident HF not preceded by clinical myocardial infarction (75%). Among African Americans, a greater proportion of HF risk (68% vs. 49% among Whites) is caused by modifiable risk factors, including elevated systolic blood pressure, hyperglycemia, coronary heart disease, left ventricular hypertrophy (LVH), and smoking. LVH was three times more common in African Americans than in Whites (Benjamin et al., 2020).
African American patients are also more likely to be readmitted to the hospital within 30 days of admission than White or Hispanic patients. The presence of asymptomatic LV systolic dysfunction was higher in African Americans (2.7%) than in Whites, Chinese, and Latinx combined (1.7%). The following graph shows the preponderance of HF in the African American community compared to Whites, regardless of gender (Benjamin et al., 2020)
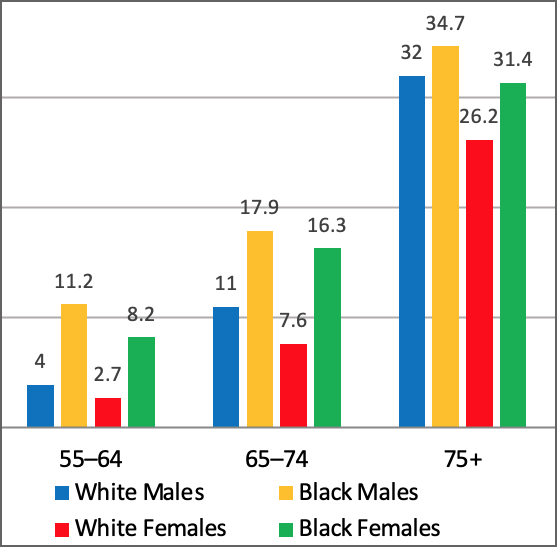
First acute decompensated heart failure annual event rates per 1,000 person years by age, sex, and race, United States, 2005–2014. (Adapted from: Atherosclerosis Risk in Communities [ARIC] Study.)
Gender
Men are diagnosed more frequently with systolic HF; women are diagnosed more frequently with diastolic HF. Men with HF benefit more from ACE inhibitors; women with HF are more likely to have the ACE inhibitor–related cough as a persistent side effect (Harding et al., 2020).
Men are diagnosed more frequently with systolic HF due to higher prevalence of coronary artery disease (CAD). Women develop HF at an older age than men. Women are more likely to be diagnosed with diastolic HF due to a higher prevalence of hypertension. Women with HF are also more likely to have CAD, diabetes, valvular disease, and depression (Cleveland Clinic, 2019).