EXPOSURE PREVENTION
It is important for all healthcare workers to understand the role they play in protecting themselves, coworkers, patients, and families from exposure to bloodborne pathogens. The employer’s exposure control plan provides the following detailed information about how each healthcare worker can take appropriate steps to reduce or eliminate the risk of exposure to bloodborne pathogens as well as other infectious agents.
Universal and Standard Precautions
Universal Precautions is the term used to describe a prevention strategy in which all blood and OPIM are treated as if they are actually infectious, regardless of the perceived status of the source individual. In other words, whether or not one thinks the blood/body fluid is infected with bloodborne pathogens, treat it as if it is. This approach is used in all situations where exposure to blood or OPIM is possible. In addition, it means that certain engineering and work practice controls are always utilized in situations where exposure may occur.
OSHA’s Bloodborne Pathogens Standard allows for healthcare facilities to use acceptable alternatives to Universal Precautions. The CDC revised the infection control practice from Universal Precautions to Standard Precautions in 1996. Standard Precautions combine the major features of Universal Precautions with Body Substance Isolation (BSI). Standard Precautions incorporate not only the fluids and materials covered by the Bloodborne Pathogens Standard but expand coverage to include any and all body fluids and substances (OSHA, 2012).
These precautions are intended to address all modes of transmission by any type of organism. Routes of transmission include:
- Contact (direct or indirect):
- Direct contact is transfer of microorganisms from one infected person to another without a contaminated intermediate object or person (e.g., blood splatter).
- Indirect contact involves transfer of an infectious agent though a contaminated intermediate object or person (e.g., needlestick, other sharp object). Contaminated hands of healthcare personnel are important contributors to indirect contact transmission.
- Droplet: Transmission of infection (e.g., coronavirus, influenza virus) traveling directly from the respiratory tract of infectious individuals to susceptible mucosal surfaces of the recipient, generally over short distances, necessitating facial protection.
- Airborne: Transmission by dissemination of either airborne droplet nuclei or small particles containing infectious agents (e.g., Myobacterium tuberculosis) that remain infective over time and distance, requiring the use of special air handling and ventilation systems.
(CDC, 2019c)
Standard Precautions for Bloodborne Pathogens
The Standard Precautions that are to be followed by all healthcare workers when concerned with bloodborne pathogens or other potentially infectious materials include:
- Performing hand hygiene
- Using personal protective equipment (PPE) whenever there is an expectation of possible exposure to infectious material
- Following respiratory hygiene/cough etiquette principles
- Ensuring appropriate patient placement
- Properly handling and properly cleaning and disinfecting of patient care equipment and instruments/devices; appropriate cleaning and disinfecting of the environment
- Handling textiles and laundry carefully
- Wearing a surgical mask when performing lumbar punctures
- Ensuring healthcare safety by proper handling of regulated waste, including proper handling of needles and other sharps
(CDC, 2019d)
HAND HYGIENE
Hand hygiene is the first line of defense, the single most important practice in preventing the spread of infectious agents. Hand hygiene in Standard Precautions means cleaning the hands with either soap and water, antiseptic hand wash/rub, or surgical hand antisepsis. Hand hygiene is done to reduce the spread of potentially infectious agents from healthcare workers to patients and from patients to healthcare workers.
The CDC advises healthcare workers who are delivering healthcare to avoid unnecessary touching of surfaces in close proximity to the patient to prevent both contamination of clean hands from environmental surfaces and transmission of pathogens from contaminated hands.
Hand hygiene should be performed:
- Before eating
- Before and after having direct contact with a patient’s intact skin
- After contact with blood, body fluids or excretions, mucous membranes, nonintact skin, or wound dressings
- After contact with inanimate objections (including medical equipment) in the immediate vicinity of the patient
- When hands will be moving from a contaminated body site to a clean body site during patient care
- After glove removal
- After using a restroom
(CDC, 2019d)
Recommendations regarding fingernails state:
- Healthcare providers should not wear artificial fingernails or extensions when having direct contact with patients at high risk (e.g., those in ICU or ORs). Pathogens can live under artificial fingernails both before and after use of an alcohol-based hand sanitizer and handwashing.
- Keep natural nail tips less than 1/4-inch long.
HAND HYGIENE WITH SOAP AND WATER OR HAND SANITIZER
The CDC guidelines for hand hygiene in healthcare settings recommend:
When using soap and water:
- Wet hands with clean running water (warm or cold) and apply the amount of product recommended by the manufacturer to hands.
- Lather hands by rubbing them together. Lather the back of the hands, between fingers, and under nails.
- Scrub hands for 15 to 20 seconds.
- Rinse hands well under clean running water.
- Dry hands using a disposable towel. Use a clean disposable towel to turn off the faucet.
When using an alcohol-based hand sanitizer:
- Apply the amount of product recommended by the manufacturer to the palm of one hand.
- Rub hands together.
- Rub the product over all the surfaces of the hands and fingers until hands are dry; this should take about 20 seconds.
(CDC, 2020e)
PERSONAL PROTECTIVE EQUIPMENT (PPE)
To protect oneself, healthcare providers must have a protective barrier between them and any potentially infectious material. Personal protective equipment is defined by OSHA as specialized clothing or equipment worn by a healthcare worker for protection against infectious materials.
Employers are required to provide and maintain clean, appropriate PPE and clothing free of charge to employees. Latex-free PPE must be made available on request. PPE must be readily accessible to employees and available in appropriate sizes. It is important to know which type of PPE is available at work and where it is stored.
Types of PPE used in healthcare settings to protect healthcare workers from exposure to bloodborne pathogens include:
- Gloves
- Gowns, aprons, coveralls, laboratory coats
- Masks, face shields, goggles
- Ventilation devices: mouthpieces, pocket masks, resuscitation devices
- Head coverings
- Boots/shoe covers
- Respirators
Factors that influence the selection of appropriate PPE include:
- Type of exposure anticipated
- Splash/spray versus touch
- Category of isolation precautions (Contact, Droplet, Airborne)
- Durability and appropriateness for the task
- Fit of the equipment
Gloves
Gloves are the most common type of PPE. They are used for patient care as well as when contacting environmental services. Gloves can be sterile or nonsterile and single use or reusable. Because of allergy concerns, latex products have been eliminated in many facilities, and materials used for gloves are mostly synthetics such as vinyl or nitrile.
Most patient care activities require the use of a single pair of nonsterile gloves. Sterile surgical gloves are worn when performing invasive patient procedures. At times two pairs of gloves may be worn for additional protection during surgical procedures. Environmental service personnel often wear reusable heavy-duty gloves to work with caustic disinfectants.
Proper glove use includes:
- Performing hand hygiene prior to donning gloves and before touching the patient or the patient environment
- Working from clean to dirty
- Limiting touch contamination (e.g., adjusting eyeglasses, touching light switches, etc.) when wearing gloves that have been in contact with a patient
- Changing gloves during use if torn, when heavily soiled, and after use on each patient
- Removing gloves carefully to avoid contamination
- Disposing of gloves in a proper receptacle
- Performing hand hygiene immediately following removal of gloves
- Never wearing the same pair of gloves in the care of more than one patient
- Never washing or reusing disposable gloves
(CDC, 2020f)
Gowns/Aprons
Gowns or aprons can be natural or human-made, reusable or disposable, resistant to fluid penetration, and clean or sterile. Sterile gowns are only required when performing invasive procedures.
Isolation gowns are preferred, but aprons occasionally are used where limited contamination is expected. Gowns should fully cover the torso, fit comfortably over the body, and have long sleeves that fit snugly at the wrist.
A waterproof apron is often worn during surgical or obstetrical procedures when a large volume of blood or body fluids are anticipated.
Proper use of gowns, aprons, and coveralls include:
- Wear a gown that is appropriate to the task to protect skin and prevent soiling or contamination of clothing.
- Wear a gown for direct patient contact if the patient has uncontained secretions or excretions.
- Remove gown and perform hand hygiene before leaving the patient’s environment.
- Do not reuse gowns, even for repeated contacts with the same patient.
(CDC, 2019d)
Mouth, Nose, and Eye Protection
Face and eye protection are used during procedures and patient care activities likely to generate splashes or sprays of blood, body fluids, secretions, or excretions. Select PPE according to the need anticipated by the task to be performed.
- Masks protect the nose and mouth and should fully cover them to prevent fluid penetration.
- Goggles protect the eyes and should fit over and around them snuggly. Personal prescription glasses are not a substitute for goggles. Some goggles have antifog features that improve clarity.
- Face shields protect the face, nose, mouth, and eyes. A face shield should cover the forehead, extend below the chin, and wrap around the sides of the face.
(CDC, 2019d)
Head Coverings
Head coverings such as surgical caps are worn when gross contamination is expected, such as during orthopedic surgery or autopsies (OSHA, 2012).
Boots/Shoe Covers
Theater boots are waterproof boots worn by surgical personnel as a protective measure from contamination with blood and other body fluids. Shoe covers protect the wearer from accidental spills and bodily fluids (OSHA, 2012).
PUTTING ON PPE
There are various ways to put on PPE. Training and practice using the healthcare facility’s procedure is critical. The CDC recommends that PPE be put on (donned) in the following sequence:
- Gown
- Mask or N95 filtering respirator
- Face shield or goggles
- Gloves
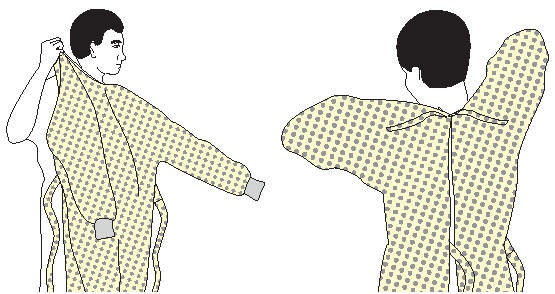
How to put on a gown:
- Select appropriate type and size.
- Perform hand hygiene using hand sanitizer.
- Put on with opening in the back.
- Secure at neck and waist.
- If gown is too small, use two gowns, with the first tied in front, the second tied in back.
How to put on a respirator:
- Respirator straps should be placed on the crown of the head (top strap) and base of the neck (bottom strap). Perform a user seal check each time putting on the respirator.
How to put on a mask:
- Place over nose, mouth, and chin.
- Fit flexible nose piece over bridge of nose using both hands. Do not bend or tent. Do not pinch the nosepiece with one hand.
- Ensure facemask extends under the chin.
- Mask ties should be secured on the crown of the head (top tie) and base of the neck. If the mask has loops, hook them appropriately around the ears.
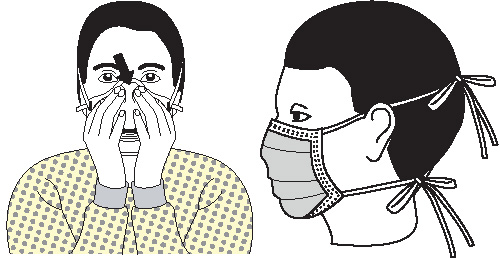
How to put on goggles and face shield:
- Place over face and eyes.
- Adjust to fit.

How to put on gloves:
- Select correct type and size.
- Insert hands into gloves.
- Extend gloves over isolation gown cuffs (wrists).
(CDC, 2020g)
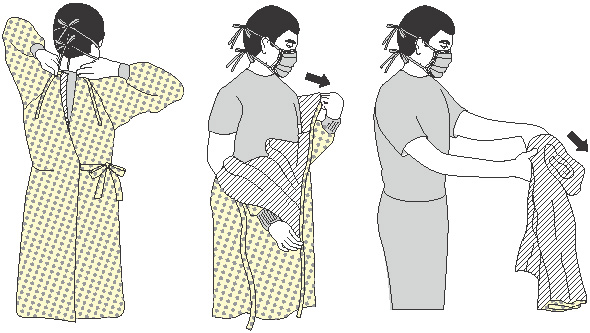
REMOVING PPE
More than one doffing method may be acceptable. Training and practice using the healthcare facility’s procedure is critical. The following is one example of doffing recommended by the CDC.
Contaminated PPE should be removed in the following sequence:
- Gloves
- Gown
- Hand hygiene and exit patient room
- Face shield or goggles
- Mask or respirator
- Hand hygiene
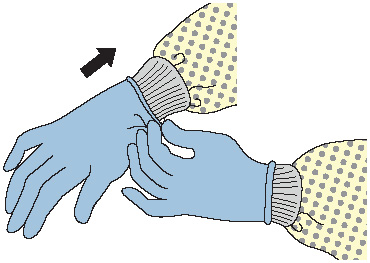
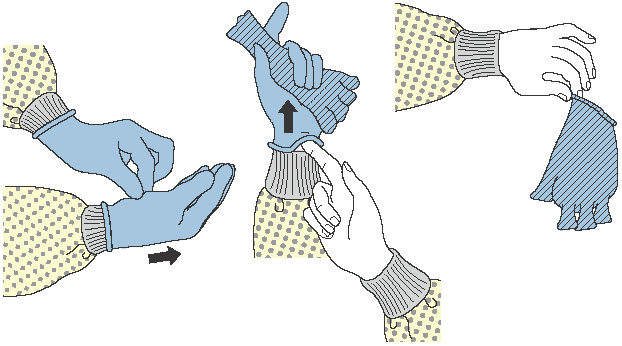
How to remove gloves:
- Grasp outside edge near wrist.
- Peel away from hand, turning glove inside out.
- Hold in opposite gloved hand.
- Slide ungloved finger under wrist of remaining glove.
- Peel off from inside, creating a bag for both gloves.
- Discard.
- Perform hand hygiene if contamination occurs.
How to remove gown:
- Consider gown front and sleeves to be contaminated.
- Unfasten ties. (Some gown ties can be broken rather than untied.)
- Peel gown away from neck and shoulders, touching inside of gown only.
- Turn contaminated outside toward the inside.
- Fold or roll into a bundle and discard.
- Perform hand hygiene before exiting the patient area.
How to remove goggles or face shield:
- Consider outside of goggles or face shield to be contaminated.
- Grasp ear- or headpieces from the back with ungloved hands by lifting head band or ear pieces.
- Lift away from face.
- Place in designated receptacle for reprocessing or disposal.
- Perform hand hygiene if contamination occurs.

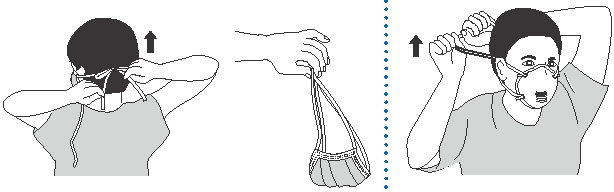
How to remove mask or respirator:
- Consider front of mask or respirator to be contaminated; do not touch.
- Respirator: Remove the bottom strap of the respirator by touching only the strap and bringing it carefully over the head. Grasp the top strap and bring it carefully over the head. Then pull the respirator away from the face without touching the front of it.
- Facemask: Carefully untie (or unhook from the ears) and pull away from face without touching the front.
- Discard.
- Perform hand hygiene.
(CDC, 2020g)
ENHANCED PRECAUTIONS AGAINST EBOLA VIRUS TRANSMISSION
The CDC provides guidance for healthcare workers who are caring for a person with confirmed Ebola or persons under investigation for Ebola. This guidance recommends:
- Healthcare workers caring for patient with Ebola or persons under investigation for Ebola are required to receive comprehensive training and have demonstrated competency in performing Ebola-related infection control practices and procedures.
- Personal protective equipment that covers the clothing and skin and completely protects mucous membranes is required:
- A disposable impermeable gown extending to at least mid-calf or disposable coverall, preferably without a hood. Coveralls with or without integrated socks are acceptable.
- Disposable apron covering the torso to level of mid-calf should be used over the gown or coveralls if the patient is vomiting or has diarrhea. An apron should be used routinely if the facility is using a coverall that has an exposed, unprotected zipper in the front.
- Disposable examination gloves with extended cuffs. Two pairs of gloves should be worn so that a heavily soiled outer glove can be removed and replaced safely during care.
- Disposable boot covers that extend to at least mid-calf. Disposable ankle-high shoe covers (surgical booties) worn over boot covers may also be considered.
- An N-95 respirator with a disposable surgical hood extending to the shoulders and fully covering the neck. Alternatively, a PAPR can be used that includes a full face shield, helmet, or headpiece and disposable hood.
- Full face shield.
When personnel are providing care to patients with Ebola, they must be supervised by an on-site manager at all times, and a trained observer must supervise each step of every PPE donning/doffing procedure to make certain established PPE protocols are completed correctly (CDC, 2018).
CLEANING AND DISINFECTING
All equipment and environmental and working surfaces must be cleaned and decontaminated after contact with blood or other potentially infectious material. Protective gloves and other PPE should be worn as necessary, and an appropriate disinfectant should be used. Such disinfections can be a diluted bleach solution or EPA-registered antimicrobial products such as tuberculocides, sterilants, or products registered against HIV/HBV.
When cleaning up a blood spill or OPIM, use protective gloves or other PPE as necessary and:
- Confine the spill and immediately wipe up the spill with paper towels or other disposable absorbent material and discard the contaminated materials in an appropriate, labeled infectious waste container.
- Clean up all blood thoroughly using neutral detergent and warm water solution before applying the disinfectant.
- Apply facility-approved intermediate-level disinfecting solution onto all contaminated areas of the surface.
- When using a diluted bleach solution, contact time is the length of time it takes for the solution to dry. (Do not use a diluted bleach solution to clean up a urine spill due to risk of chlorine gas.)
- Allow disinfectant to remain wet on the surface for the recommended contact time, then rinse the area with clean water to remove the disinfectant residue (if required).
- Immediately send all reusable supplies and equipment (e.g., cleaning cloths, mops) for reprocessing (i.e., cleaning and disinfection) after the spill is cleaned up.
Liquid chlorine bleach comes in different concentrations. To make a 0.5% chlorine solution from 3.5% bleach, use 6 parts of water for each part bleach (CDC, 2020h).
HANDLING CONTAMINATED LAUNDRY
Contaminated laundry (i.e., soiled with blood or OPIM or that may contain sharps) should be handled as little as possible with a minimum of agitation. Contaminated laundry is bagged at the location of use into labeled or color-coded bags or containers. Contaminated laundry that is wet is placed and transported in containers or bags that prevent soak-through or leakage. Contaminated laundry should not be rinsed at the location of use.
Avoid uniform contamination by holding soiled laundry away from the body, and do not hold laundry bags close to the body or squeeze them when transporting to avoid punctures from improperly discarded sharps (OSHA, 2012).
HANDLING REGULATED WASTE
Regulated waste refers to:
- Any liquid or semi-liquid blood or other OPIM
- Contaminated items that would release blood or OPIM in a liquid or semi-liquid state if compressed
- Items that are caked with dried blood or OPIM and are capable of releasing these materials during handling
- Contaminated sharps
Regulated waste should be placed in strong, leak-proof plastic bags or a container capable of being autoclaved and should be properly labeled or color-coded (OSHA, 2012).
Sharps Handling
Contaminated sharps are needles, blades (such as scalpels), scissors, and other medical instruments and objects that can puncture the skin. Contaminated sharps must be properly disposed of immediately or as soon as possible into containers that are closable, puncture-resistant, leak-proof on the sides and bottom, and color-coded or labeled with a biohazard symbol.
HOW TO HANDLE SHARPS
- Discard needle/syringe units without attempting to recap the needle whenever possible.
- If a needle must be recapped, never use both hands. Use the single-hand “scoop” method.
- Never break or shear needles.
- To move or pick up needles or other sharp devices, use a mechanical device or tool, such as forceps, pliers, or broom and dustpan.
- Dispose of needles in labeled sharps containers only; sharps containers must be accessible and maintained upright. When transporting sharps containers, close the containers immediately before removal or replacement to prevent spillage or protrusion of contents during handling or transport.
- Fill a sharps container up to the fill line or two thirds full. Do not overfill the container.
(OSHA, 2012)