BARRIERS AND PERSONAL PROTECTIVE EQUIPMENT
Personal protective equipment (PPE) includes a variety of barriers and respirators used alone or in combination to protect mucous membranes, airways, skin, and clothing from contact with infectious agents. The selection of PPE is based on the nature of the patient interaction and/or the likely mode or modes of transmission.
Types of Personal Protective Equipment
PPE must be readily accessible to employees and available in appropriate sizes. It is important to know which type of PPE is available at work and where it is stored. To protect themselves, healthcare providers must have a barrier between them and any potentially infectious material.
Types of PPE used in healthcare settings include:
- Gloves
- Gowns/aprons/coveralls
- Face and eye protection
- Head coverings
- Boots/shoe covers
- Respirators
Factors that influence the selection of appropriate PPE include:
- Type of exposure anticipated:
- Blood or body fluid splash/spray vs. touch
- Contact with minimal bleeding/drainage/body substances
- Contact with large volume bleeding/drainage/body substances that are likely to soak through the contact area
- Category of isolation precautions (Contact, Droplet, Airborne)
- Durability and appropriateness for the task. This affects whether a gown or fluid-proof apron is selected, or if a gown is selected, whether it must be fluid-resistant, fluid-proof, or neither.
- Fit of the equipment. The employer must ensure that all PPE are available in sizes appropriate for the workforce to be protected.
(See also “Standard Precautions” earlier in this course for additional information related to PPE.)
GLOVES
Gloves are the most common type of PPE. They are used for patient care as well as environmental service. Gloves can be sterile or nonsterile and single use or reusable. Because of allergy concerns, latex products have been eliminated in many facilities, and materials used for gloves are mostly synthetics such as vinyl or nitrile.
Gloves can protect both patients and healthcare personnel from exposure to infectious material that may be carried on the hands. Nonsterile disposable medical gloves are available for routine patient care. The selection of glove type for nonsurgical use is based on the task that is to be performed and anticipated contact with chemicals and chemotherapeutic agents.
For contact with blood and body fluids during nonsurgical patient care, a single pair of gloves provides adequate barrier protection. However, there is considerable variability among gloves, and studies have shown repeatedly that vinyl gloves have higher failure rates than latex or nitrile gloves. For this reason, either latex or nitrile gloves are preferable for clinical procedures that require manual dexterity and/or will involve more than brief patient contact.
Most patient-care activities require the use of a single pair of nonsterile gloves. Vinyl gloves are frequently available and work well if patient contact is limited. However, some gloves do not provide a snug fit on the hand, especially around the wrist, and should be not used if extensive contact is likely. Gloves should not tear or damage easily and must stand up to the task.
Sterile surgical gloves are worn when performing invasive patient procedures. At times, two pairs of gloves may be worn during surgical procedures for additional protection.
Heavier, reusable utility gloves are indicated for non-patient-care activities such as handling or cleaning contaminated equipment or surfaces. Environmental service personnel often wear reusable heavy-duty gloves to work with caustic disinfectants.
Proper glove use includes:
- Performing hand hygiene before putting on gloves
- Putting gloves on last when being worn in combination with other PPE
- Working from clean to dirty
- Limiting touch contamination (e.g., adjusting eyeglasses, touching light switches, etc.) when wearing gloves that have been in contact with a patient
- Changing gloves during the care of a single patient to prevent cross-contamination of body sites or if patient interaction also involves touching portable keyboards or other mobile equipment that is transported from room to room
- Changing gloves during use if torn or when heavily soiled and after use on each patient
- Discarding gloves between patients and disposing of gloves in proper receptacle
- Performing hand hygiene following glove removal
- Never washing or reusing disposable gloves
(CDC, 2019c)
GOWNS/APRONS
Clinical and laboratory coats or jackets worn over personal clothing are not considered PPE.
Isolation gowns are preferred, but aprons occasionally are used where limited contamination is expected. Gowns must fully cover the torso, fit comfortably over the body, and have long sleeves that fit snugly at the wrist.
The type of protection is based on the nature of the patient interaction, including the anticipated degree of contact with infectious material and potential for blood and body fluid penetration of the barrier. Clean gowns are generally used for isolation precautions. Sterile gowns are needed only when performing invasive procedures.
For prevention of transmission of an infectious agent, donning of both gown and gloves upon room entry is indicated. Gowns are always worn in combination with gloves and with other PPE when indicated, and are usually the first piece of PPE to be donned. Full coverage of arms and body front from neck to the mid-thigh or below ensures that clothing and exposed body areas are protected.
FACE AND EYE PROTECTION
Face and eye protection are used during patient-care activities that are likely to generate splashes or sprays of blood, body fluids, secretions, or excretions. Two mask types are available for use: surgical masks and procedure or isolation masks.
Masks are used for three primary purposes:
- Worn by healthcare personnel to protect from contact with infectious material from patients
- Worn by healthcare personnel who are engaged in procedures requiring sterile technique to protect patients from exposure to infectious agents carried in the healthcare worker’s mouth or nose
- Placed on patients to limit potential dissemination of infectious respiratory secretions from the patient to others
Eye protection depends on the circumstances of exposure, other PPE used, and personal vision needs. Goggles protect the eyes and should fit over and around them snuggly. Personal prescription glasses are not a substitute for goggles. Some goggles have antifog features that improve clarity, and many styles of goggles fit adequately over prescription lenses with minimal gaps.
Face shields protect the face, nose, mouth, and eyes. A face shield should cover the forehead, extend below the chin, and wrap around the sides of the face. Face shields can be worn along with face masks.
Removal of a face shield, goggles, and mask can be performed safely after removing gloves and performing hand hygiene (CDC, 2019c).
HEAD COVERINGS
Head coverings such as surgical caps are worn when gross contamination is expected, such as during orthopedic surgery or autopsies (OSHA, 2012).
BOOTS/SHOE COVERS
Theater boots are waterproof boots worn by surgical personnel as a protective measure from contamination with blood and other body fluids. Shoe covers protect the wearer from accidental spills and body fluids (OSHA, 2012).
RESPIRATORY PROTECTION
Respiratory protection includes both surgical and standard N95 or higher-level respirators. Respirators require medical evaluation to determine if it is safe for the healthcare worker to wear one and to fit the worker with the appropriate respirator size and type. Healthcare workers are responsible for performing a user-seal check (formerly called a “fit check”) each time a respirator is donned to minimize air leakage around the face piece.
A surgical N95 respirator is recommended only for use by healthcare personnel who need protection from both airborne and fluid hazards such as splashes and sprays.
The CDC currently recommends standard N95 or higher-level respirators for healthcare personnel who are exposed to patients with suspected or confirmed tuberculosis and COVID-19 (Siegel et al., 2019; CDC, 2020j).
Putting On and Removing PPE
PUTTING ON PPE
There are various ways to put on PPE. Training and practice using the healthcare facility’s procedure is critical. The CDC recommends that PPE be put on (donned) in the following sequence:
- Gown
- Mask or N95 filtering respirator
- Face shield or goggles
- Gloves
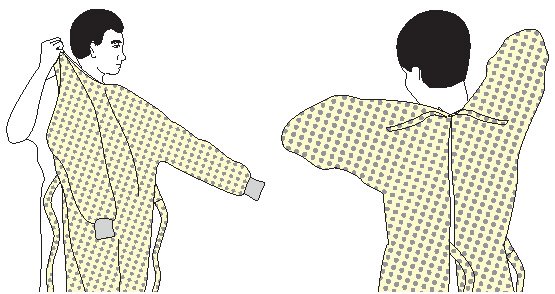
How to put on a gown:
- Select appropriate type and size.
- Perform hand hygiene using hand sanitizer.
- Put on with opening in the back.
- Secure at neck and waist.
- If gown is too small, use two gowns, with the first tied in front, the second tied in back.
How to put on a respirator:
- Respirator straps should be placed on the crown of the head (top strap) and base of the neck (bottom strap). Perform a user seal check each time putting on the respirator.
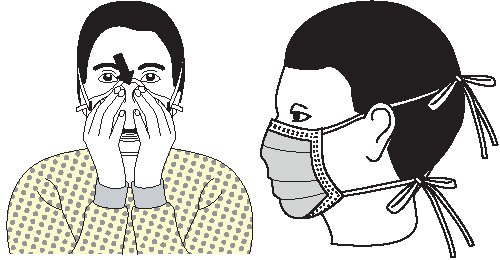
How to put on a mask:
- Place over nose, mouth, and chin.
- Fit flexible nose piece over bridge of nose using both hands. Do not bend or tent. Do not pinch the nosepiece with one hand.
- Ensure facemask extends under the chin.
- Mask ties should be secured on the crown of the head (top tie) and base of the neck. If the mask has loops, hook them appropriately around the ears.
How to put on goggles and face shield:
- Place over face and eyes.
- Adjust to fit.

How to put on gloves:
- Select correct type and size.
- Insert hands into gloves.
- Extend gloves over isolation gown cuffs (wrists).
(CDC, 2020k)
REMOVING PPE
More than one doffing method may be acceptable. Training and practice using the healthcare facility’s procedure is critical. The following is one example of doffing recommended by the CDC.
Contaminated PPE should be removed in the following sequence:
- Gloves
- Gown
- Hand hygiene and exit patient room
- Face shield or goggles
- Mask or respirator
- Hand hygiene
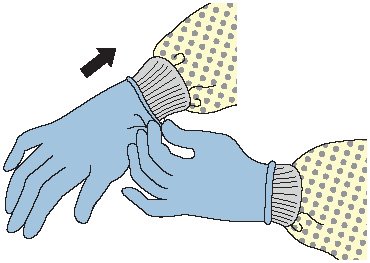
How to remove gloves:
- Grasp outside edge near wrist.
- Peel away from hand, turning glove inside out.
- Hold in opposite gloved hand.
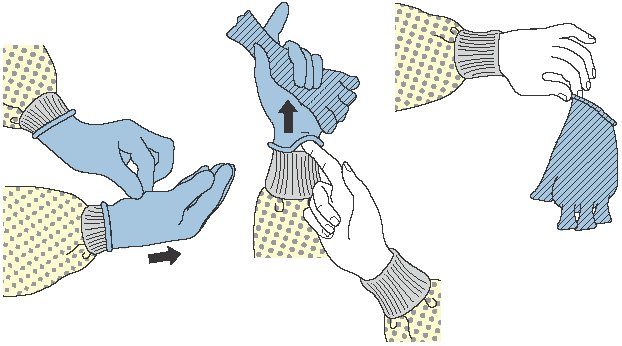
- Slide ungloved finger under wrist of remaining glove.
- Peel off from inside, creating a bag for both gloves.
- Discard.
- Perform hand hygiene if contamination occurs.
How to remove gown:
- Consider gown front and sleeves to be contaminated.
- Unfasten ties. (Some gown ties can be broken rather than untied.)
- Peel gown away from neck and shoulders, touching inside of gown only.
- Turn contaminated outside toward the inside.
- Fold or roll into a bundle and discard.
- Perform hand hygiene before exiting the patient area.

How to remove goggles or face shield:
- Consider outside of goggles or face shield to be contaminated.
- Grasp ear- or headpieces from the back with ungloved hands by lifting head band or ear pieces.
- Lift away from face.
- Place in designated receptacle for reprocessing or disposal.
- Perform hand hygiene if contamination occurs.

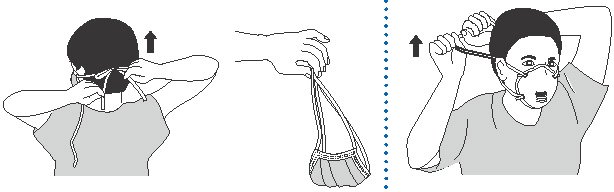
How to remove mask or respirator:
- Consider front of mask or respirator to be contaminated; do not touch.
- Respirator: Remove the bottom strap of the respirator by touching only the strap and bringing it carefully over the head. Grasp the top strap and bring it carefully over the head. Then pull the respirator away from the face without touching the front of it.
- Facemask: Carefully untie (or unhook from the ears) and pull away from face without touching the front.
- Discard.
- Perform hand hygiene.
(CDC, 2020k)
PERSONAL PROTECTIVE EQUIPMENT AND SARS-CoV-2 (COVID-19) PANDEMIC
- Healthcare personnel should adhere to Standard and Transmission-based Precautions when caring for patients with SARS-CoV-2 infection.
- Transmission-based Precautions for SARS-CoV-2 require the use of a filtering facepiece respirator (e.g., N95).
- A study has found that SARS-CoV-2 is able to survive on materials such as plastic, stainless steel, and cardboard for up to 72 hours.
- In the event of PPE shortages, the CDC recommends that each healthcare worker be issued five respirators. They will wear one respirator each day and store it in a breathable paper bag at the end of each shift. The order of use should be repeated with a minimum of five days between each use.
- Ultraviolet germicidal irradiation, vaporous hydrogen peroxide, and moist heat have shown the most promise as methods to decontaminate respirators.
- Reuse of respirators should only be practiced where shortages exist.
(CDC, 2020l)
(See also “Resources” at the end of this course for a link to the latest CDC guidance on PPE and COVID-19.)