METHODS FOR PREVENTING THE SPREAD OF PATHOGENS IN HEALTHCARE SETTINGS
Preventing the spread of pathogens involves breaking one of the links of the chain of infection, and the link most amenable to actions by healthcare workers are modes of transmission.
Standard Precautions
One of the most effective infection control practices is Standard Precautions. Standard Precautions are a set of infection control practices used to prevent transmission of pathogens and are based on the concept that all blood, body fluids, nonintact skin (including rashes), and mucous membranes may contain transmissible pathogens. Standard Precautions are implemented for all patient care settings and include:
- Performing hand hygiene
- Use of personal protective equipment (PPE) whenever there is an expectation of possible exposure to infectious material
- Following respiratory hygiene/cough etiquette principles
- Ensuring appropriate patient placement
- Proper handling and proper cleaning and disinfecting of patient-care equipment and instruments or devices
- Cleaning and disinfecting the environment appropriately
- Handling textiles and laundry carefully
- Following safe injection practices
- Wearing a surgical mask when performing lumbar punctures
- Ensuring healthcare worker safety, including handling of needles and other sharps
(CDC, 2019c)
BLOOD AND OTHER POTENTIALLY INFECTIOUS MATERIAL (OPIM)
All occupational exposures to blood or other potentially infectious materials place healthcare providers at risk for infection with bloodborne pathogens. Standard Precautions are designed to eliminate exposure to blood and other potentially infectious material.
OSHA defines blood as:
- Human blood
- Human blood components
- Products made from human blood
OPIM include:
- Semen
- Vaginal secretions
- Cerebrospinal fluid
- Synovial fluid
- Pleural fluid
- Pericardial fluid
- Peritoneal fluid
- Amniotic fluid
- Saliva in dental procedures
- Any body fluids that are visibly contaminated with blood
- All body fluids in situations where it is difficult or impossible to differentiate between them
- Any unfixed tissue or organ (other than intact skin) from a human (living or dead)
- HBV- and HIV-containing cell or tissue cultures, organ cultures, and HBV- or HIV-containing culture medium or other solutions
- Blood, organs, or other tissues from experimental animals infected with HBV or HIV
(OSHA, 2012; CDC, 2020g)
HAND HYGIENE
Hand hygiene is the single most important practice to reduce transmission of infectious agents and means cleaning hands by using handwashing with soap and water, antiseptic hand wash, antiseptic hand rub, or surgical hand antisepsis.
During delivery of healthcare, the CDC (2020h) advises healthcare workers to avoid unnecessary touching of surfaces in close proximity to the patient and requires performance of hand hygiene in accordance with the following recommendations:
Wash hands with soap and water:
- When hands are visibly soiled
- After caring for a person with known or infectious diarrhea
- After known or suspected exposure to spores (e.g., B. anthracis, C. difficile outbreaks)
Unless hands are visibly soiled, an alcohol-based hand sanitizer is the method of choice for hand hygiene. Alcohol-based hand rubs come in gel, rinse, wipe, and foam form. They are less drying and have superior microbicidal activity in comparison to soap and water. Indications include:
- Immediately before having direct contact with a patient’s intact skin (e.g., taking a pulse)
- Before performing an aseptic task (e.g., placing an indwelling device) or handling invasive medical devices
- Before moving from work on a soiled body site to a clean body site on the same patient
- After touching a patient or the patient’s immediate environment
- After contact with blood, body fluids or excretions, mucous membranes, nonintact skin, or wound dressing
- After contact with inanimate objects in the immediate vicinity of the patient, including medical equipment
- Before donning gloves
- Immediately after glove removal
Skin and Nails
The CDC offers the following recommendations to maintain hand skin health:
- Use lotions and creams to prevent and decrease healthcare provider skin dryness related to frequent hand hygiene.
- Use only hand lotions approved by the healthcare facility so as to avoid interfering with hand sanitizing products.
Recommendations regarding fingernails state:
- Healthcare providers should not wear artificial fingernails or extensions when having direct contact with patients at high risk (e.g., those in ICU or ORs). Pathogens can live under artificial fingernails both before and after use of an alcohol-based hand sanitizer and handwashing.
- Keep natural nail tips less than 1/4-inch long.
(CDC, 2020h)
Some studies have shown that more pathogens are present on the skin underneath rings than comparable areas of skin on fingers without rings. Rings may also increase the risk of glove tears. However, further studies are needed to determine if wearing rings results in an increased spread of pathogens (CDC, 2020h).
Studies regarding the issue of wearing nail polish remain inconclusive. Bacterial burden increases over time for natural nails, standard nail polish, and gel polish. However, reductions in the bacterial burden of natural nails and standard polish, but not gel polish, has occurred following hand hygiene, indicating that gel polish may be more difficult to clean using alcohol hand gel (Hewlett et al., 2018).
It appears that wearing a simple finger band and unchipped nail polish may be acceptable, although removal of all rings and wearing no nail polish may be the safest prevention option.
Hand Cleansing Techniques
Both the CDC and the World Health Organization provide guidelines in the techniques of handwashing as well as hand rub cleansing using an alcohol hand sanitizer.
Handwashing requires 15 to 20 seconds to be effective (about as long as it takes to sing “Happy Birthday” twice).
Technique for handwashing with soap and water (WHO, 2020b.):
Handrub technique using alcohol hand sanitizer (WHO, 2009):

Apply a palmful of the product in a cupped hand.

Rub hands palm to palm.
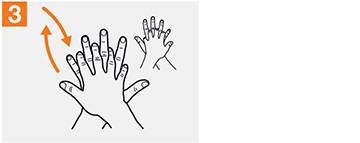
Rub palm over left dorsum with interlaced fingers and vice versa.

Rub palm to palm with fingers interlaced.
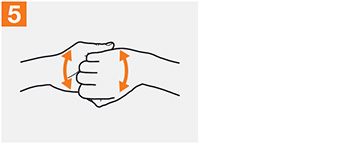
Rub backs of fingers to opposing palms with fingers interlocked.

Rub left thumb rotationally clasped in right palm and vice versa with right thumb in left palm.
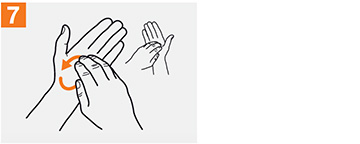
Rub clasped fingers of right hand rotationally, backwards, and forwards in left palm and vice versa with left fingers in right palm.

Once dry, hands are safe.
Surgical Hand Antisepsis
Performing surgical hand antisepsis using either an antimicrobial soap or an alcohol-based hand sanitizer with persistent activity is recommended before donning sterile gloves when performing surgical procedures.
- Remove rings, watches, and bracelets before beginning to scrub.
- Clean under nails using a nail cleaner under running water.
- When using antimicrobial soap, scrub hands and forearms for 2 to 6 minutes. Long scrub times (e.g., 10 minutes) are not necessary.
- When using an alcohol-based surgical hand-scrub product with persistent activity, follow the manufacturer’s instructions.
- When using an alcohol-based surgical hand-scrub, prewash hands and forearms with a nonantimicrobial soap and dry hands and forearms completely before donning sterile gloves.
- Double gloving is advised during invasive procedures that pose an increased risk of exposure to blood.
(CDC, 2020h)
GLOVES
The CDC recommendations state that gloves should be worn according to Standard Precautions, as described below:
- Make sure that gloves fit properly before performing any tasks.
- Wear disposable medical examination gloves for providing direct patient care.
- Wear disposable medical examination gloves or reusable utility gloves for cleaning the environment or medical equipment.
- Gloves should be worn when it can be reasonably anticipated that contact with blood or other potentially infectious materials, mucous membranes, nonintact skin, potentially contaminated skin, or contaminated equipment could occur.
- Wearing gloves is not a substitute for hand hygiene.
- Hand hygiene should be performed immediately after removing gloves.
- Prior to a task that requires gloves, perform hand hygiene before donning them and before touching the patient or the patient environment.
- Change gloves and perform hand hygiene during patient care if:
- Gloves become damaged
- Gloves become visibly soiled with blood or body fluids following a task
- Moving from work on a soiled body site to a clean body site on the same patient or if another clinical indication for hand hygiene occurs
- Never wear the same pair of gloves in the care of more than one patient.
- Do not touch the face when wearing gloves.
- Do not wear gloves in the halls, except as approved by facility.
(CDC, 2020h)
EYE PROTECTION, MASKS, FACE SHIELDS, AND GOWNS
Appropriate barriers include personal protective equipment used alone or in combination to protect the mucous membranes, airway, skin, and clothing from contact with infectious materials. These barriers include eye protection, face masks, and gowns.
- Eye protection (goggles and face shields) should be worn when there is a potential of a splash or spray of blood, respiratory secretions, or other body fluids. Personal eyeglasses and contact lenses are not considered adequate eye protection.
- Select masks, goggles, face shields, and combinations of each according to the need anticipated by the task to be performed.
- A mask should be worn to protect patients from exposure to infectious agents carried in the mouth or nose of healthcare personnel. A mask should be worn when placing a catheter or injecting material into the spinal canal or subdural space, or to perform intrathecal chemotherapy.
- A fluid resistant, nonsterile gown should be worn to protect skin and clothing during procedures or activities where contact with blood or body fluids is anticipated.
- A new gown should be worn for the care of each individual patient.
- A gown should be worn prior to direct patient contact that may generate splashes or sprays of blood, body fluids, secretions, and excretions.
- Remove gown and perform hand hygiene before leaving the patient’s environment.
- Do not reuse gowns, even for repeated contacts with the same patient.
(WDHS, 2018; CDC, 2019c)
CASE
Sharon is a nurse working the night shift in respiratory ICU. Her assignment for the night includes three patients. As her shift begins, Sharon must first check in on her patient who is intubated and perform tracheotomy care and suctioning. Sharon recognizes that the suctioning procedure may expose her to the patient’s secretions. Considering which level of Standard Precautions to apply, she dons appropriate PPE, which includes a gown, gloves, mask, and goggles. After caring for the patient, she disposes properly of all PPE and washes her hands prior to moving on to care for her next patient.
RESPIRATORY HYGIENE/COUGH ETIQUETTE
To prevent transmission of all respiratory infections in healthcare settings, Standard Precautions require that the following infection control measures be implemented at the point of initial encounter with patients or accompanying individuals who have signs and symptoms of respiratory infection:
- Educate healthcare workers on the importance of source-control methods to contain respiratory secretions, especially during outbreaks of respiratory illness such as influenza, measles, or coronavirus.
- Post signs at entrances and in strategic places, such as elevators and cafeterias, in both ambulatory and inpatient settings in languages appropriate to the population served, with instructions to patients and other persons on cough etiquette.
- Make the following supplies readily available:
- Tissues
- No-touch waste containers
- Hand hygiene supplies and instructions (alcohol-based hand rub, sinks when available)
- For patients with signs and symptoms of respiratory infection, offer a mask to contain their secretions.
- Separate patients with symptoms of respiratory infection from the general patient population by 6 feet.
- For healthcare workers, wear a surgical or procedural mask whenever in close proximity to a patient with signs or symptoms of respiratory infection.
(CDC, 2019c)
COUGH ETIQUETTE
- Cover the mouth and nose when coughing and/or sneezing with a tissue; if no tissue is available, cough or sneeze into the elbow, not the hands.
- Immediately dispose of the tissue into the nearest waste container.
- Perform hand hygiene after coughing, sneezing, or using a facial tissue.
(CDC, 2019c)
PATIENT-CARE EQUIPMENT AND INSTRUMENTS/DEVICES
The following policies and procedures are recommended for containing, transporting, and handling patient-care equipment and instruments/devices that may be contaminated with blood or body fluids.
- Meticulously clean patient-care items with water and detergent or with water and enzymatic cleaners before high-level disinfection or sterilization procedures.
- Remove visible organic residue (e.g., blood and tissue) and inorganic salts with appropriate effective cleaning agents.
- Clean medical devices as soon as practical after use to avoid soiled materials drying onto the instruments. Dried or baked materials make the removal process more difficult and disinfection or sterilization less effective or ineffective.
- Wear PPE, such as gloves and gown, according to the level of expected contamination when handling patient-care equipment and instruments/devices that are visibly soiled or may have been in contact with blood or body fluids.
(CDC, 2019d)
CARE OF THE ENVIRONMENT
Policies and procedures for keeping the environment clean include using facility-approved disinfectants to clean patient equipment and to clean high-touch surfaces on a more frequent schedule, including:
- Bedrails
- IV poles
- Sink handles
- Bedside tables
- Counters where medications and supplies are prepared
- Edges of privacy curtains
- Patient monitoring equipment (keyboards, control panels)
- Transport equipment (wheelchair handles)
- Call bells
- Doorknobs
- Light switches
- Surfaces in and around toilets in patients’ rooms
Spills of blood or other potentially infectious materials must be promptly cleaned and decontaminated following proper procedures and using protective gloves and other personal protective equipment appropriate for the task (CDC, 2019d).
In facilities providing healthcare to pediatric patients or that have waiting areas with child play toys, policies and procedures for cleaning and disinfecting toys at regular intervals should follow these principles:
- Select play toys that can easily be cleaned and disinfected and avoid use of stuffed, furry toys if they will be shared.
- Clean and disinfect large stationary toys (e.g., climbing equipment) at least weekly and whenever visibly soiled.
- If toys are likely to be put in the mouth, rinse with water after disinfection; alternatively, wash in a dishwasher.
- When a toy requires cleaning and disinfection, do so immediately or store in a designated, labeled container separate from toys that are clean and ready for use.
Include multiuse electronic equipment in environmental cleaning and disinfection policies, especially those items used by patients, those used during delivery of patient care, and mobile devices that are moved in and out of patient rooms frequently (CDC, 2019d).
TEXTILES AND LAUNDRY
Recommendations include:
- Handle used textiles and fabrics with minimum agitation to avoid contamination of air, surfaces, and persons.
- Bag or otherwise contain contaminated textiles and fabrics at the point of use.
- Use leak-resistant containment for textiles and fabrics contaminated with blood or body substances.
- If laundry chutes are used, ensure they are properly designed, maintained, and used so as to minimize dispersion of aerosols from contaminated laundry.
(CDC, 2019d)
PATIENT PLACEMENT
Include the potential for transmission of infectious agents in patient-placement decisions.
- Place patients who pose a risk for transmission to others in a single-patient room when available (e.g., those with uncontained secretions, excretions, or wound drainage; infants with suspected viral respiratory or gastrointestinal infections).
- Determine patient placement based on the following principles:
- Route(s) of transmission of known or suspected pathogen
- Risk factors for transmission in the infected patient
- Risk factors for adverse outcomes resulting from an HAI in other patients in the area or room being considered for patient placement
- Availability of single-patient rooms
- Patient options for room sharing (e.g., cohorting patients with the same infection)
(CDC, 2019c)
SAFE INJECTION PRACTICES
The following recommendations apply to the use of needles, cannulas that replace needles, and where applicable, intravenous delivery systems.
- Use aseptic technique to avoid contamination of sterile injection equipment.
- Do not administer medications from a syringe to multiple patients.
- Needles, cannulas, and syringes are single-patient-use items; they should not be reused to access a medication or solution that might be used for a subsequent patient.
- Use IV bags, tubing, and connectors for one patient only and dispose appropriately after use.
- Do not use bags or bottles of intravenous solution as a common source of supply for multiple patients.
- Consider a syringe or needle/cannula to be contaminated after it has entered an IV bag or administration set.
- Use single-dose vials whenever possible.
- Do not use one single-dose vial or ampule for several patients or combine contents of several vials.
- If multidose vials must be used, use only a sterile needle/cannula and syringe to access them.
- Do not keep multidose vials in the immediate patient-care areas; store as recommended by the manufacturer and discard if sterility is compromised.
(CDC, 2019c)
(See also “Sharps- and Injection-Related Practices and Controls” later in this course.)
INFECTION CONTROL PRACTICES FOR LUMBAR PUNCTURE PROCEDURES
Healthcare workers should wear a surgical mask when placing a catheter or injecting material into the epidural or subdural spaces to prevent infection caused by the transfer through normal breathing or coughing of oral flora to the central nervous system of the patient during the procedure (CDC, 2019c).
Transmission-Based Precautions
In addition to Standard Precautions, which are used with all patients, patients with documented or suspected infection or colonization with highly transmissible or epidemiologically important pathogens require additional precautions known as transmission-based precautions. The duration of these precautions is to be extended for immunosuppressed patients with viral infections due to prolonged shedding of viral agents that may be transmitted to others. There are three types of transmission-based precautions: Contact, Droplet, and Airborne.
CONTACT PRECAUTIONS
Contact Precautions are designed to minimize transmission of organisms that are easily spread by contact with hands or objects. Conditions requiring Contact Precautions may include:
- Enteric infections (C. diff., E. coli)
- Viral infections (rhinovirus, COVID-19)
- Scabies
- Impetigo
- Enteric infections
- Noncontained abscesses or decubitus ulcers (S. aureus, Group A Streptococcus)
(Anderson, 2020)
CDC Contact Precautions are summarized below:
Patient Placement
In acute care hospitals, place the patient in a single-patient room when available. When a single-patient room is not available:
- Prioritize patients with conditions that may facilitate transmission (e.g., stool incontinence) for single-patient-room placement.
- Place together in the same room (cohort) patients who are infected or colonized with the same pathogen and are suitable roommates.
- If necessary to place the patient in a room with a patient who is not infected or colonized with the same pathogen:
- Avoid placement in rooms with patients whose conditions increase risk of adverse outcome or that may facilitate transmission (e.g., immunocompromised, open wounds, or have anticipated prolonged lengths of stay).
- Ensure physical separation of greater than 3 feet. Draw privacy curtain between beds.
- Change protective attire and perform hand hygiene between contacts with patients in the same room.
In long-term care and other residential settings, make decisions about placement on a case-by-case basis, balancing risk to other patients in the room, presence of risk factors increasing likelihood of transmission, and potential adverse psychological impact on infected or colonized patient.
In ambulatory settings, place patients in an examination room or cubicle as soon as possible.
Use of Personal Protective Equipment
- Don gloves upon entry into the room or cubicle.
- Wear gloves whenever touching the patient’s intact skin or surfaces and articles in close proximity to the patient.
- Wear a gown when anticipating clothing will have direct contact with the patient or potentially contaminated environmental surfaces or equipment in close proximity to the patient.
- Don a gown upon entry and remove and perform hand hygiene before leaving the patient-care area.
- After removal of gown, ensure clothing and skin do not contact environmental surfaces in the patient-care area.
Patient Transport
- In acute care hospitals and long-term care and other residential settings, limit transport and movement of patients outside of the room to medically necessary purposes.
- If necessary to transport or move, ensure infected or colonized areas of the patient’s body are contained and covered.
- Remove and dispose of contaminated PPE and perform hand hygiene prior to transporting.
- Don clean PPE to handle the patient at the transport destination.
Patient-Care Equipment and Instruments/Devices
- Handle equipment and instruments/devices according to Standard Precautions.
- In acute care hospitals, long-term care, and other residential settings, use disposable equipment (e.g., blood pressure cuffs) or implement patient-dedicated use. If common use is unavoidable, clean and disinfect before use on another patient.
- Limit the amount of nondisposable patient-care equipment brought into the patient’s home. Whenever possible, leave equipment in the home until discharge from home services.
- If noncritical equipment (e.g., stethoscope) cannot remain, clean and disinfect items before taking them from the home using a low- to intermediate-level disinfectant. Alternatively, place in a plastic bag for transport and later cleaning and disinfection.
- In ambulatory settings, place contaminated reusable noncritical patient-care equipment in a plastic bag for transport to a soiled utility area for reprocessing.
- Ensure that rooms of patients are prioritized for frequent cleaning and disinfection (at least daily), with a focus on frequently touched surfaces (e.g., bed rails, over-bed table, bedside commode, lavatory, doorknobs) and equipment in the immediate vicinity of the patient.
(CDC, 2019c)
CASE
Mrs. Alberts is a patient on the hospital surgical unit who is recovering from a complicated hip replacement surgery. She has been on antibiotics during the pre- and post-operative periods. On day four, she develops watery diarrhea, which tests positive for C. difficile.
The nurse initiates Contact Precautions and communicates with Mrs. Albert’s physician to confirm the order. Contact Precautions require all visitors and care providers to wear a gown and gloves when entering the patient’s room. Mrs. Alberts will also need to have disposable or dedicated equipment that is used only for her, such as a blood pressure cuff, stethoscope, and other equipment that may be needed for her care.
DROPLET PRECAUTIONS
Droplet Precautions are designed to prevent transmission of diseases easily spread by large-particle droplets (>5 microns in size) produced when the patient coughs, sneezes, or talks, or during the performance of procedures. Conditions requiring Droplet Precautions may include:
- Neisseria meningitidis infection
- Mycoplasma pneumoniae infection
- Pertussis (whooping cough) (Bordetella pertussis)
- Influenza
- Rubella
- Mumps
- Adenovirus infection
- Parvovirus B19 infection
- Rhinovirus infection
- Certain coronavirus infections (e.g., MERS-CoV, SARS-CoV, and SARS-CoV-2)
(Anderson, 2020)
CDC Droplet Precautions are summarized below:
Patient Placement
In acute care hospitals, place the patient in a single-patient room when available. When a single room is not available:
- Prioritize patients who have excessive cough and sputum production for single-room placement.
- Place together in the same room (cohort) patients who are infected with the same pathogen.
- If necessary to place a patient in a room with another patient who does not have the same infection:
- Avoid placing in the same room with patients who have conditions that may increase risk of adverse outcome or who may facilitate transmission (e.g., those who are immunocompromised or have anticipated prolonged lengths of stay).
- Ensure patients are physically separated greater than 3 feet and draw a privacy curtain between beds to minimize close contact.
- Change protective attire and perform hand hygiene between contact with patients in the same room, regardless of whether one patient or both patients are on Droplet Precautions.
In long-term care and other residential settings, make decisions on a case-by-case basis following consideration of infection risks to other patients in the room and available alternatives.
In ambulatory settings, place patients in an examination room or cubicle as soon as possible.
Instruct all patients to follow respiratory hygiene/cough etiquette.
Use of Personal Protective Equipment
Wear a mask upon entry into the patient room or cubicle.
Patient Transport
- In acute care hospitals, long-term care facilities, and other residential settings, limit transport and movement outside the room to medically necessary purposes.
- If transporting or moving is necessary, instruct the patient to wear a mask and follow respiratory hygiene/cough etiquette.
- No mask is required for persons transporting patients.
(CDC, 2019c)
RECOMMENDED INFECTION PREVENTION AND CONTROL PRACTICES FOR COVID-19
The CDC recommends using additional infection prevention and control practices along with Standard and Transmission-Based Precautions when caring for patients with suspected or confirmed SARS-CoV-2 infection. These include, but are not limited to:
- Implement telehealth and nursing-directed triage protocols.
- Screen and triage everyone entering a healthcare facility for signs and symptoms of COVID-19.
- Perform screening assessments of all admitted patients on a daily basis.
- Implement universal source control measures (cloth face coverings or facemask) for everyone in a healthcare facility.
- Ensure all healthcare personnel wear a facemask at all times in all places within the healthcare facility.
- Ensure all healthcare personnel wear eye protection in addition to a facemask during patient care encounters to ensure protection.
- Encourage physical distancing (6 feet) between people.
- Limit visitors to only those essential for patients’ physical and emotional well-being and care.
(Due to the rapidly growing body of knowledge concerning SARS-CoV-2 infection, it is recommended that all healthcare professionals review the most recent infection control guidelines provided by the CDC. See “Resources” at the end of this course.)
(CDC, 2020i)
AIRBORNE PRECAUTIONS
Airborne Precautions are designed to prevent transmission of small particles of respiratory secretions that contain infectious microbes over time and long distances. Airborne Precautions are the only type that requires a negative-pressure airborne infection isolation room (AIIR) with door kept closed and use of an N95 respirator.
Conditions requiring Airborne Precautions may include:
- Tuberculosis
- Varicella
- Measles
- Smallpox
- Certain coronavirus infections (e.g., MERS-CoV, SARS-CoV, and SARS-CoV-2)
- Ebola
(Anderson, 2020)
CDC Airborne Precautions are summarized below.
Patient Placement
- In acute care hospitals and long-term care settings, place patients in an AIIR that has been constructed in accordance with current guidelines.
- Keep the AIIR door closed except for entry and exit.
- When an AIIR is not available, transfer patient to a facility that has an available AIIR.
- In the event of an outbreak or exposure involving large numbers of patients requiring Airborne Precautions:
- Consult infection control professionals.
- Cohort patients presumed to have the same infection in areas away from other patients.
- Use temporary portable solutions (e.g., exhaust fan) to create negative pressure in the converted environment, and discharge air directly to the outside or through HEPA filters before it is introduced to other air spaces.
- In ambulatory settings:
- Develop a system (e.g., signage, triage) to identify patients requiring Airborne Precautions.
- Place in an AIIR as soon as possible. If not available, put a surgical mask on the patient, instruct in respiratory hygiene/cough etiquette, and place in an examination room. Once the patient leaves, the room should remain vacant for about one hour to allow full exchange of air.
- Instruct patients to wear a surgical mask and observe respiratory hygiene/cough etiquette. Once in an AIIR, mask may be removed.
- Restrict susceptible healthcare personnel from entering rooms of patients known to have measles (rubeola), varicella (chickenpox), disseminate zoster, or smallpox if other immune healthcare personnel are available.
- Respiratory protection is recommended for all healthcare personnel, vaccinated and unvaccinated.
Use of Personal Protective Equipment
- Wear a fit-tested NIOSH-approved N95 or higher-level respirator when entering the room or home of a patient with known or confirmed infectious pulmonary tuberculosis and when procedures for treating tuberculosis skin lesions are performed that would aerosolize viable organisms.
Patient Transport
- In acute care hospitals, long-term care, and other residential settings, limit transport and movement outside of the room to medically necessary purposes.
- If transport or movement is necessary, instruct patients to wear a surgical mask and observe respiratory hygiene/cough etiquette. Cover infectious skin lesions.
- Transporting healthcare personnel do not need to wear a mask or respirator during transport if patient is wearing a mask and infectious skin lesions are covered.
Exposure Management
- Healthcare workers are encouraged to be vaccinated against common childhood illnesses to prevent outbreaks in vulnerable populations such as neonates.
- Annual influenza vaccination reduces the incidence of institutional outbreaks.
- Healthcare workers should receive periodic boosters against pertussis.
- Immunize or provide appropriate immune globulin to susceptible persons as soon as possible following unprotected exposure to a patient with measles, varicella, or smallpox.
(CDC, 2019c)