HIV/AIDS Training and Education for Healthcare Professionals
CONTACT HOURS: 6
Copyright © 2020 Wild Iris Medical Education, Inc. All Rights Reserved.
LEARNING OUTCOME AND OBJECTIVES: Upon completion of this course, you will have increased your knowledge of HIV/AIDS in order to better care for your patients. Specific learning objectives to address potential learning gaps include:
- Discuss the etiology and epidemiology of HIV in the United States.
- Summarize the factors and risks for transmission of HIV in general and among healthcare workers in particular.
- Identify preventive and control measures for HIV/AIDS.
- Discuss accepted procedures and regulations for HIV testing and counseling.
- Describe the clinical manifestations and treatment guidelines for HIV/AIDS.
- Explain legal and ethical issues related to HIV/AIDS.
- Summarize the psychosocial issues associated with HIV/AIDS.
TABLE OF CONTENTS
- Etiology and Epidemiology of HIV/AIDS
- Transmission and Infection Control
- HIV Testing and Counseling
- Clinical Manifestations and Treatment of HIV and AIDS
- Legal and Ethical Issues
- Psychosocial and Mental Health Issues
- Conclusion
- Resources
- References
ETIOLOGY AND EPIDEMIOLOGY OF HIV/AIDS
HIV, the human immunodeficiency virus, is a virus that spreads via certain body fluids and specifically attacks the CD4+ or T cells of the immune system. CD4+ T cells are also called helper T cells. They are the cornerstones of both inflammatory and regulatory responses of our immune system. T cells are lymphocytes that are predominantly produced in the thymus and play a key role in the immune system’s defense of the body against infection. As time passes, the virus can destroy so many of these specialized cells that the immune system no longer is able to fight off infections and disease.
HIV is unique among many other viruses because the body is unable to destroy the HIV completely, even with treatment. As a result, once a person is infected with the virus, the person will have it for the remainder of their life (CDC, 2019a).
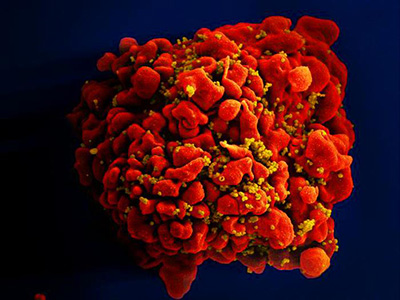
A single T cell (red) infected by numerous, spheroid shaped HIV particles (yellow). (Source: National Institute of Allergy and Infectious Diseases, 2012.)
After the initial infection and without treatment, the virus continues to multiply, and over a period of time (which can be ten years or longer), common opportunistic infections (OIs) begin to take advantage of the body’s very weak immunity. Common OIs can be life-threatening and may include:
- Cryptococcal meningitis
- Toxoplasmosis
- Pneumocystis pneumonia
- Esophageal candidiasis
- Certain cancers, such as Kaposi’s sarcoma
Once they have such an opportunistic infection, the person now is considered to have AIDS, acquired immunodeficiency syndrome, the most advanced stage of the HIV infection (NIAID, 2019).
Origin and Strains of HIV
DNA analysis has identified the HIV-1 virus as originating in a strain of chimpanzees in Kinshasa, in the Democratic Republic of Congo, around 1920. Chimpanzees were hunted for food, and it is believed that the simian (chimpanzee) version of the virus was most likely transmitted to humans following contact with the animal’s infected blood after ingestion of the meat. The simian immunodeficiency virus then mutated into the human form of the virus. HIV has existed in the United States at least since the mid to late 1970s (CDC, 2019a; Avert, 2019a).
HIV, like other viruses, changes over time, resulting in different strains (genetic variants or subtypes) of the virus. There are two main types of HIV: HIV-1 and HIV-2. HIV-1 is the most common, while HIV-2 is less common and accounts for fewer infections. The strains of HIV-1 can be classified into four groups: M, N, O, and P. The N, O, and P strains are quite uncommon, while group M is responsible for approximately 95% of all infections worldwide.
In 2020 a new strain of HIV was found for the first time in nearly 20 years. The newly discovered strain is part of group M and has been labelled as sub-type L. This new strain is important, but it does not pose a new public health threat since it occurs rarely and can be effectively treated with existing antiretrovirals (Yamaguchi et al., 2020).
Disease Pathogenesis
HIV is unable to grow or reproduce on its own and depends on a host cell for the raw materials and energy necessary for all the biochemical activities that allow the virus to reproduce. In order to accomplish this, it must locate and bind to a specific type of cell, a CD4+ T cell.
CD4+ T cells (or T-helper cells) are the cornerstones of both the inflammatory and regulatory responses of the immune system. They are a class of white blood cells that help other lymphocytes (memory B cells) that are responsible for remembering an antigen and producing an antibody to fight it based on stored data following exposure to it in the past.
Once the virus binds to the cell, it then enters the cell and eventually takes control of the cell’s DNA and begins to replicate itself. This leaves the T cell unable to perform its vital function as part of the immune system. The new HIV particles are then released from the cell into the bloodstream, where the process begins again in other T cells (Cachay, 2019).
Following transmission of the virus, the individual will typically progress through three stages of the illness.
- Stage 1: Acute infection is the earliest stage, when seroconversion takes place, and the person is very contagious.
- Stage 2: Clinical latency is a stage that can last for 10 or 15 years, during which time immunosuppression gradually develops. The person may be asymptomatic and can transmit the virus to others.
- Stage 3: AIDS is the final, severe stage of HIV infection, at which point the immune system is severely damaged and opportunistic infections or cancers begin to appear.
Epidemiology
Approximately 1.1 million people in the United States are living with HIV. From 2010 to 2017, the annual number of new HIV diagnoses decreased 9%. In 2018, there were an estimated 38,000 new HIV infections. Trends varied for different groups of people.
In 2018, 17,032 people in the United States and six dependent areas received a stage 3 (AIDS) diagnosis, and in 2017 there were 16,350 deaths (due to any cause) among adults and adolescents with a diagnosis of HIV (CDC, 2019b; HIV.gov, 2020a).
Gay and bisexual men are the population most affected by HIV. In 2018, they accounted for 69% of all HIV diagnoses:
- HIV diagnoses among Black/African American gay and bisexual men remained stable.
- HIV diagnoses among White gay and bisexual men decreased 19%.
- HIV diagnoses among Hispanic/Latino gay and bisexual men increased 27%.
Heterosexuals and people who inject drugs also continue to be affected. In 2018:
- Heterosexuals accounted for 24% of HIV diagnoses, with men accounting for 7% and women for 16%.
- People who inject drugs accounted for 7% of HIV diagnoses, men 4% and women 3%.
By race/ethnicity, Blacks/African Americans and Hispanics/Latinos are disproportionately affected by HIV.
- Blacks/African Americans comprise 13% of the population and accounted for 42% of new diagnoses.
- Hispanics/Latinos comprise 18% of the population and accounted for 27% of new HIV diagnoses.
HIV DIAGNOSES BY RACE/ETHNICITY, 2018
- 43% Black/African American
- 26% Hispanic/Latino
- 26% White
- 2% Asian
- <1% American Indian/Alaska Native
- <1% Native Hawaiian/Other Pacific Islander
- 3% Multiple races
(CDC, 2019b)
Across U.S. states and regions, there was an uneven distribution of new HIV diagnoses in 2018. The South had the highest percentage (51%), followed by the West (20%), the Northeast (16%), and the Midwest (13%).
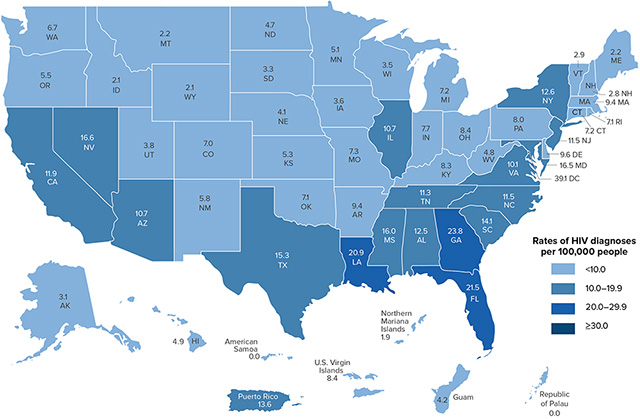
Rates of new HIV diagnoses per 100,000 people, 2018. (Source: CDC, 2019b.)