STAGING PRESSURE INJURIES
Pressure injuries are staged to classify the degree of tissue damage that is present. The staging system was originally created in 1975 as a means to describe the amount of anatomical tissue loss in a pressure injury. The use of stages in pressure injury assessment is a way to classify the amount and type of tissue destroyed based on anatomic depth. Having and using a common classification system allows all clinicians a way of communicating accurately about what is wrong. It is only used to describe pressure injuries, not other wounds.
The clinician must first determine the etiology of the injury being assessed and the presence of pressure and/or shear. If these factors are not present, the injury is not a pressure injury. First, the injury is cleansed to remove loose debris and to validate the etiology is pressure or shear; then the staging system is used to stage the injury appropriately. When labeling a pressure injury, it is important to use correct anatomical terms to identify its location on the body.
Stage 1 Pressure Injury
A stage 1 pressure injury is indicated by intact skin with a localized area of nonblanchable erythema, usually over a bony prominence. Darkly pigmented skin may not have visible blanching; its color may differ from the surrounding area. Presence of blanchable erythema or changes in sensation, temperature, or firmness may precede visual changes. Color changes in stage 1 pressure injuries do not include purple or maroon discoloration; these may instead indicate deep tissue pressure injury (see “Deep Tissue Pressure Injury” below).
Blanchable erythema (redness) means that when the red area is compressed by the finger, the area turns white or pale and the redness returns when the pressure is released. Nonblanchable erythema means the area under the finger remains red as it is compressed. Nonblanchable redness indicates that tissue damage has already occurred.
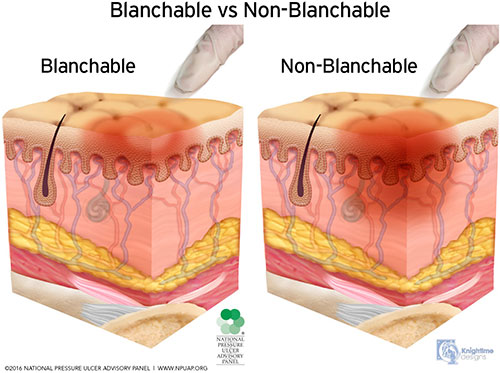
Blanchable vs. nonblanchable erythema. (Source: © NPUAP, used with permission.)
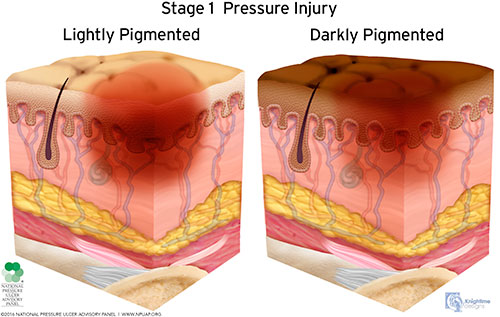
(Source: © NPUAP, used with permission.)

Stage 1 pressure injury on a patient’s buttocks/coccyx. (Source: © 2011, Gordian Medical, Inc., dba American Medical Technologies, used with permission.)
TERMINOLOGY
- Slough is a soft, moist, avascular tissue. It may be white, yellow, tan, or green; loose or firmly adherent; and described as resembling chicken fat.
- Eschar is black or brown necrotic tissue. It can be loose or firmly adherent; hard, soft, or boggy; and look like a scab, although there is no healing occurring beneath it.
- Undermining is tissue destruction to underlying, intact skin along the wound edges.
- Tunneling is a path of tissue destruction that occurs in any direction from the surface or edge of the wound.
(See also wound injury images below.)
Stage 2 Pressure Injury
A stage 2 pressure injury is indicated by partial-thickness loss of skin with exposed dermis (see images). The wound bed is viable, pink, or red; moist; and may also present as an intact or ruptured serum-filled blister. Adipose (fat) and deeper tissues are not visible. Granulation tissue, slough, and eschar are not present. These injuries commonly result from adverse microclimate and shear in the skin over the pelvis and shear in the heel.
It is especially important that the presence or history of pressure and/or shear be confirmed in a suspected stage 2 pressure injury. This stage should not be used to describe moisture-associated skin damage (MASD), including incontinence associated dermatitis (IAD), intertriginous dermatitis (rashes in skin folds), medical adhesive–related skin injury, or traumatic wounds (skin tears, burns, abrasions).
Stage 2 pressure injuries heal by reepithelialization and not by granulation tissue formation (i.e., by return of intact skin and not by scarring). At times the superficial fascia under the dermis is visible and evident as a thin, ivory-colored, nonremovable layer. A viable dermis is pink or red, shiny, and blanchable; it is not granular.
“Partial thickness” means that the damage is confined to the epidermis and/or dermis but does not penetrate below the dermis.
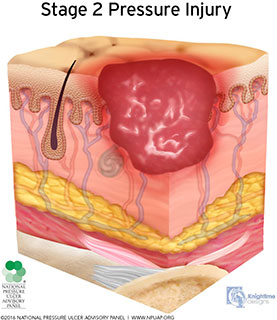
Note reddened wound edges. (Source: © NPUAP, used with permission.)

Stage 2 pressure injury on a patient’s buttocks/coccyx area. (Source: © 2011, Gordian Medical, Inc., dba American Medical Technologies, used with permission.)
Stage 3 Pressure Injury
A stage 3 pressure injury is indicated by full-thickness loss of skin in which adipose (fat) is visible in the ulcer and granulation tissue and epibole (rolled wound edges) are often present (see images). Slough and/or eschar may be visible. Undermining and tunneling may occur. Fascia, muscle, tendon, ligament, cartilage, and/or bone are not exposed. When slough or eschar obscures the extent of tissue loss, the injury is considered unstageable.
The depth of a stage 3 pressure injury varies by anatomical location. The bridge of the nose, ear, occiput, and malleolus do not have subcutaneous tissue, and stage 3 injuries here will be shallow. In contrast, areas of significant fat deposits can develop extremely deep stage 3 pressure injuries. Accurate staging is based on assessment of the extent of damage and the visible tissue layer, not depth.
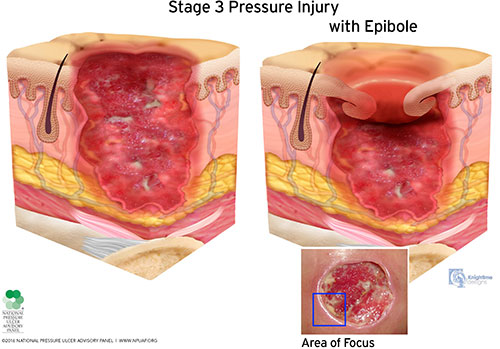
(Source: © NPUAP, used with permission.)

Stage 3 pressure injury on a patient’s ankle. (Source: © 2011, Gordian Medical, Inc., dba American Medical Technologies, used with permission.)
Stage 4 Pressure Injury
A stage 4 pressure injury is indicated by full-thickness skin and tissue loss with exposed or directly palpable fascia, muscle, tendon, ligament, cartilage, or bone in the ulcer (see images). Slough and/or eschar may be visible. Epibole (rolled edges), undermining, and/or tunneling often occur. Depth varies by anatomical location. As bone may be in the ulcer, clinicians should consider the presence of osteomyelitis in stage 4 pressure injuries. When slough or eschar obscures the extent of tissue loss, the injury is considered unstageable.
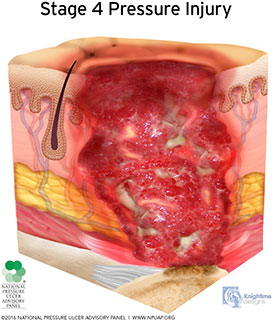
(Source: © NPUAP, used with permission.)

Stage 4 pressure injury on a patient’s ankle. (Source: © 2011, Gordian Medical, Inc., dba American Medical Technologies, used with permission.)
Unstageable Pressure Injury
An unstageable pressure injury is indicated by full-thickness skin and tissue loss in which the extent of tissue damage within the pressure injury cannot be confirmed because it is obscured by slough or eschar (see images). If slough and eschar is removed, a stage 3 or stage 4 pressure injury will be revealed because slough and/or eschar do not form in stage 1 or 2 injuries.
Clinicians should bear in mind that “unstageable” refers to the inability to visualize the wound base rather than the clinician’s inability to determine the injury stage.
Stable eschar (i.e., dry, adherent, intact without erythema or fluctuance) on the heel or ischemic limb should not be softened or removed. Stable eschar acts as the body’s natural or biological cover dressing. Removing stable eschar in the poorly perfused area results in an open wound that may expose the body to infection and decrease the ability to heal. Treat stable eschar on a poorly perfused area as dry gangrene; do not moisten or soften it. The most important intervention when managing this type of injury is pressure redistribution rather than eschar removal. As the eschar loosens from the wound bed, trim the edges to avoid inadvertent removal.

(Source: © NPUAP, used with permission.)

Unstageable pressure ulcer. (Source: © AAWC, used with permission.)
Deep Tissue Pressure Injury
A deep tissue pressure injury (DTPI) is indicated by intact or nonintact skin with localized area of persistent nonblanchable, deep red, maroon, purple discoloration or epidermal separation revealing a dark wound bed or blood-filled blister (see images). Pain and temperature change often precede skin color changes. Discoloration may appear differently in darkly pigmented skin. DTPI is not used to describe vascular, traumatic, neuropathic, or dermatologic conditions.
This injury results from intense and/or prolonged pressure and shear forces at the bone-muscle interface. The wound may evolve rapidly to reveal the actual extent of tissue injury, or may resolve without tissue loss. If necrotic tissue, subcutaneous tissue, granulation tissue, fascia, muscle, or other underlying structures are visible, this indicates a full-thickness pressure injury (unstageable, stage 3, or stage 4).
It must be confirmed that the purple skin (appearing as ecchymoses or bruising) is due to pressure or shear and not a response to medication or trauma. Identifying the timing and setting of the pressure/shear that led to the deep tissue pressure injury will help in analyzing the cause. Documentation includes the evolution of the injury after discovery (sloughing of the epidermis that reveals deeper tissue damage) and, if injury becomes full thickness, the stage of the resultant injury.
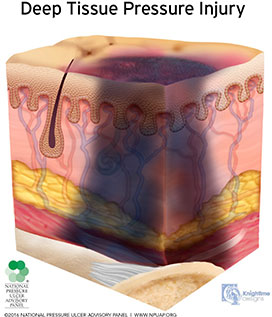
(Source: © NPUAP, used with permission.)

Deep tissue pressure injury. (Source: © 2011, Gordian Medical, Inc., dba American Medical Technologies, used with permission.)
Additional Pressure Injury Definitions
The National Pressure Injury Advisory Panel (2016a) has also defined two additional types of pressure injuries, described below.
MEDICAL DEVICE–RELATED PRESSURE INJURY
Medical device–related pressure injuries (MDRPIs) result from the use of devices designed and applied for diagnostic or therapeutic purposes. The resultant pressure injury generally conforms to the pattern or shape of the device. The injury should be staged using the same staging system.
The skin must be examined under the device. Some devices are easily removed or moved for assessment; others may require two people to assist, such as under a tracheostomy if the patient is agitated and likely to grab at the device. Pressure reduction under a medical device can occur when thin dressings are applied between the device and the skin. These dressings (thin silicone foams, hydrocolloids, etc.) should be applied before the device is applied, as it may be difficult to lift the device later to apply the dressing.
This type of wound should be documented, for example, as “stage 4 pressure injury on bridge of nose from a medical device.” The name of the device should be included in documentation to allow for analysis of the injury.
Research has shown that MDRPIs develop more quickly than pressure injuries not caused by medical devices. The most common sites for MDRPIs are the ears and feet (Kayser et al., 2018).
MUCOSAL MEMBRANE PRESSURE INJURY
Mucosal membrane pressure injury is found on mucous membranes with a history of a medical device in use at the location of the injury (see image). Mucosal tissues are especially vulnerable to pressure from medical devices such as oxygen tubing, endotracheal tubes, bite blocks, nasogastric tubes, urinary catheters, and fecal containment devices.
Because the staging system for pressure injuries is based on the anatomy of the skin, it cannot be used to stage mucosal pressure injuries. Nonblanchable erythema cannot be seen in mucous membranes; shallow open ulcers indicating superficial skin loss in the epithelium are so shallow that the naked eye cannot distinguish them from deeper, full-thickness ulcers.
The injured mucosal membrane is often inflamed and may be tender and edematous. It does not form slough or eschar. Scars do not form in mucous membranes. The medical device should be repositioned to reduce pressure. Stabilizing systems can be used to hold tubes in place without pressure.
Since the staging system cannot be used, the clinician should document the pressure injury as a “mucosal membrane tissue injury” on the body area (lip, urethra, nares, tongue, labia, etc.) and document the name of the actual device that caused the injury.
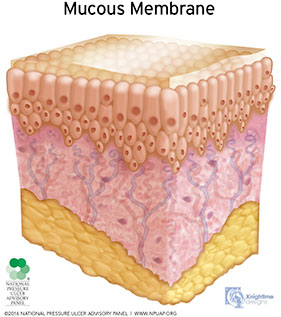
Mucosal membrane pressure injury. (Source: © NPUAP, used with permission.)
Reverse Staging
The term reverse staging came about in the 1980s as a way of describing improvement in a pressure injury. However, this term does not accurately describe what is physiologically occurring in the injury. Because staging is used only to describe the amount and type of tissue destroyed based on anatomic depth, it cannot be used to describe healing. (Documentation should not include reverse staging.)
As a pressure injury heals, it does decrease in depth, but the body does not replace the lost bone, muscle, subcutaneous fat, or dermis. Instead, the full-thickness injury is filled with granulation, or scar tissue, and then covered with new epithelium. Even a partial-thickness stage 2 injury does not return to the nonblanchable redness of a stage 1 injury. A stage 4 pressure injury that has closed should be classified as a closed stage 4 pressure injury. If a pressure ulcer reopens in the same anatomical site, the ulcer resumes the previous staging diagnosis—once a stage 4, always a stage 4 (EPUAP/NPIAP/PPPIA, 2019).
EARLIER CLARIFICATIONS TO NPIAP GUIDELINES
On January 24, 2017, the NPIAP (then NPUAP) issued “Position Statement on Staging—2017 Clarifications” to address the many requests it had received for clarification of its 2016 pressure injury guidelines. The statements are summarized here.
Position Statement 1: The diagnosis of a “pressure injury” does not mean that the healthcare provider(s) “caused” the injury. Pressure injury simply means the tissue is injured by pressure (and/or shear). It does not assign blame or in any way imply that the injury was “caused” by anything that healthcare providers “did” or “failed to do.” The word injury occurs frequently in the medical literature (e.g., kidney injury, spinal cord injury, closed head injury) to identify the existence of tissue injury, without assigning blame.
Position Statement 2: Some pressure injuries are unavoidable despite provision of evidence-based care by the healthcare team. NPUAP has long maintained that some pressure injuries are unavoidable. Evidence must be presented to support a theory of causation based on a careful analysis of the preventive care provided (or not provided) to the individual in accordance with acceptable standards of evidence-based pressure injury prevention.
Position Statement 3: The numerical staging system does not imply linear progression of pressure injuries from stage 1 through stage 4, nor does it imply healing from stage 4 through stage 1. NPUAP has long maintained this position and issued a position statement against “down staging” as early as the year 2000.
Position Statement 4: The NPUAP Staging System classifies pressure injuries based on the type of tissue loss that can be visualized or directly palpated. Pressure injuries can be staged if the type of tissue injured can be visualized or directly palpated (as with stage 4, when exposed bone is visible or directly palpated). But because there are limitations to what can be seen, two additional options for staging are provided: 1) unstageable pressure injuries to address situations where the wound base is obscured by slough and/or eschar and 2) deep tissue pressure injury (DTPI), where the skin may be intact but is purple or maroon, indicating deeper tissue damage has occurred.
Position Statement 5: The pressure injury may be more extensive than initially apparent. The wound base and surrounding tissue should be assessed for variations in sensation, temperature, firmness, color, and any expression of drainage from surrounding tissues when palpated. Tissue surrounding the “visible injury” should be assessed for changes (e.g., pain, temperature, firmness, color, and drainage) which may alert the clinician to more extensive damage than is readily visible. Additional findings should be described and documented.
Position Statement 6: Deep tissue pressure injury (DTPI) may evolve into a full-thickness wound despite optimal care. A DTPI may evolve rapidly to reveal the actual extent of tissue injury, or may resolve without tissue loss. Off-loading the area still offers the best chance for tissue that is ischemic or injured but not infarcted.
Position Statement 7: Any pressure injury should be treated in accordance with current evidence-based practices and monitored closely for changes that require reevaluation of treatment strategies.
NPUAP Staging System revisions are designed to improve the accuracy of staging when reporting “new” or “worsening” pressure injuries. NPUAP will continue to work with CMS (Center for Medicare and Medicaid Services) on further refinements of quality measures to more accurately monitor healing versus deterioration.
(NPIAP, 2017)