PRESSURE INJURY PREVENTION
It is more cost efficient to prevent a pressure injury than to cure one. Interventions that will help the clinician prevent pressure injuries include:
- Minimizing pressure through regular repositioning
- Using a support surface for body weight distribution
- Managing incontinence to prevent skin damage from moisture
- Managing nutrition and hydration to support the body in preventing damage and healing any damage that has occurred
(Baranoski & Ayello, 2016; EPUAP/NPIAP/PPPIA, 2019)
Regular Repositioning and Early Mobilization
While the underlying cause and formation of pressure injuries is multifaceted, by definition a pressure injury cannot form without pressure on the tissue. Thus, immobility is the most significant risk for the development of pressure injuries. High pressures over bony prominences for a short time and low pressures over bony prominences for a long time are equally damaging (Baranoski & Ayello, 2016). In order to decrease the risk, it is important to reduce the time and amount of pressure the patient is exposed to.
All patients must have their positions changed on a regular schedule. How often this is done is determined by each patient’s activity/mobility level, tissue tolerance, skin condition, overall medical condition, treatment goals, type of pressure redistribution support surface used, and the comfort of the patient (Shah, 2018).
Physical therapists may be involved in all aspects of pressure injury prevention, including the initial patient assessment, evaluation of patient mobility, and recommendation and implementation of treatments. An occupational therapist can also provide interventions for transfers, skill training for mobility, and independence skills for hygiene and toileting. Skills learned from these therapists can reduce incontinence and immobility, which can reduce the risk of pressure injury development (Bryant & Nix, 2016).
INTERDISCIPLINARY APPROACH
Improving the mobility of patients, or mitigating the effects of immobility, requires the assistance of many in the healthcare team:
- Bedside clinicians: Assess for all risk factors, see that needed interventions are provided, and reassess outcomes frequently.
- Physical therapists: Evaluate functional mobility and/or provide wound evaluation/treatment for patients with potential or actual pressure injury. May provide interventions including direct wound care, optimization/maintenance of joint range of motion, strength training, seating and positioning recommendations, evaluation of support surfaces, functional mobility and/or balance training, gait training, and/or assistive device recommendations/training.
- Occupational therapists: Address lifestyle factors that can lead to increased incidence of pressure injuries, including assessing the patient’s cognitive and functional capacity and recommending adaptive equipment and interventions to meet individual patient needs.
- Medical equipment department: Determine what equipment is available for the patient.
- Social workers: Uncover what resources are available to the patient.
(Bryant & Nix, 2016)
BED-BOUND PATIENTS
For bed-bound patients, the standard “turn every two hours” may be more than adequate for some but not at all adequate for others. Evidence suggests that turning/repositioning every four hours, when combined with a pressure-redistributing mattress, is as effective for prevention of pressure injury as repositioning or turning every two hours (WOCN, 2016a).
It is important to keep in mind that when lateral rotation mattresses are used for pulmonary and cardiovascular care, such rotation does not off-load the skin; the patient must still be repositioned off the bed surface and the skin checked frequently. Lateral rotation is a characteristic of specialized mattresses that rotate a patient around a longitudinal axis in a recurring sequence. Lateral rotation places the patient in positions that maintain one lung higher than the other. The goal of lateral rotation is to prevent pneumonia, not to treat or prevent pressure injury (Baranoski & Ayello, 2016).
If the medical condition is so severe that repositioning the patient regularly is not possible, then a support surface designed to decrease pressure must be used and the patient repositioned with frequent small shifts (e.g., mini or low-angle turns, elevating heels off the bed, repositioning the head and extremities every hour, and passive range of motion). (See also “Using Support Surfaces” below.)
When turning the patient, clinicians often think that the patient must be completely over on a side. This can be difficult for the clinician/caregiver to do, is uncomfortable for the patient, can result in cardio-pulmonary compromise, and actually increases pressure on the side of the body.
Instead, frequent small position changes, rather than completely turning the patient, is faster, easier, and safer for all. Any change in position is beneficial. The patient need only be tilted to the side, no more than 30 degrees, with pillows or wedges to help support and reduce the pressure over bony prominences. A small pillow behind the shoulder or the hip alters position without having to move the entire body. Bending the knee alters the pressure on the sacrum and hip. A pillow between the knees prevents pressure when one bony prominence is lying directly on top of another. A small pillow behind the heel will elevate the heel off the surface and prevent pressure.

A small turn using a bolster can be as effective as a full turn in repositioning the patient. (Source: C. Melter.)
NPIAP provides the following general recommendations for repositioning patients in bed:
- Reposition the patient in such a way that pressure is relieved or redistributed.
- Avoid positioning the patient on bony prominences with existing nonblanchable erythema.
- Avoid subjecting the skin to pressure and shear forces and use manual handling aids to reduce friction and shear. Lift—do not drag—the patient while repositioning. Dragging the patient will cause skin damage due to friction. In most situations, simple devices like lift sheets can be used.
- Use a split-leg sling mechanical lift device when available to transfer a patient into a wheelchair or bedside chair when the patient needs total assistance to transfer. A split-leg sling incorporates wide straps that circle the legs. This device allows for comfortable positioning of the patient and has the added advantage of the patient’s knees not being pushed together, which is the typical position in a hammock sling (Preferred Health Choice, 2019).
- Do not leave moving and handling equipment under the patient after use unless the equipment is specifically designed for that purpose.
- Avoid positioning directly onto medical devices such as tubes, drainage systems, or other foreign objects.
- Do not leave the patient on a bedpan longer than necessary.
- Use principles of safe patient handling to prevent injury to both the patient and the staff.
Additional recommendations for repositioning in bed include:
- Use the 30-degree tilted side-lying position, alternating between right side, back, left side, or prone position if patient can tolerate this and the medical condition allows.
- Encourage individuals who can reposition themselves to sleep in a 30- to 40-degree side-lying position or flat in bed if not contraindicated.
- Avoid lying postures that increase pressure, such as a 90-degree side-lying position or the semi-recumbent position.
- Limit head-of-bed elevation to 30 degrees for an individual on bedrest unless contraindicated by medical condition or feeding considerations. If not contraindicated, lower the head of the bed one hour after eating or intermittent bolus tube feedings (Bryant & Nix, 2016).
- If sitting in bed is necessary, avoid head-of-bed elevation or a slouched position that places pressure and shear on the sacrum and coccyx.
For a patient with an existing pressure injury:
- Do not position the patient directly on the injury or on areas of nonblanchable redness or deep tissue injury; pressure reduces perfusion to the injured tissues and will delay healing and may cause deterioration of the wound.
- Continue to turn and reposition the patient regardless of the support surface in use.
- Inspect the skin for additional damage each time the patient is turned or repositioned.
PREVENTING HEEL PRESSURE INJURIES
The reduction of pressure and shear at the heels is very important in clinical practice. Studies indicate the heels are the most common place for the occurrence of deep tissue pressure injury (DTPI), and they are the second most common sites for the occurrence of all pressure injury (WOCN, 2016b) (see “Deep Tissue Pressure Injury” later in this course). The posterior heel sustains intense pressure even when a pressure reduction surface is used. Because the heel has so little tissue, the pressure is transmitted directly to the bone.
Ideally, heels should be free of all pressure, sometimes called “floating” the heels. Pressure can be relieved by elevating the lower leg and calf from the mattress by placing a pillow under the lower leg or using a suspension device that floats the heel. The pressure will then be spread to the lower leg, relieving the heel. The recommended position for the pillow is lengthwise under the calf, with the heel suspended off the pillow. The patient must still be turned at regular intervals to promote pulmonary, renal, and vascular function along with protecting skin integrity.
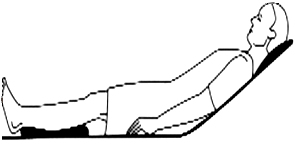
Heels are properly floated. (Source: C. Melter.)
Padding devices such as synthetic sheep skin, fleece-lined “bunny boots,” and rigid splints protect the heels and remove friction and shear but do not remove the pressure, and regular skin checks are still required. Common devices such as intravenous bags, rolled towels or sheets, cut-out rings, and water-filled gloves are not designed to redistribute pressure and can actually increase pressure.
In a small study that examined the effectiveness of several heel pressure–relieving devices, it was found that the egg-crate boot and laminated foam boot were the most effective in preventing pressure injuries.
All appropriate heel pressure–reliving devices should be used in conjunction with good nursing care, including frequent, individualized heel inspections. Patients must be reminded to promptly report any heel discomfort, and this should be followed by an immediate assessment by the clinician (Baranoski & Ayello, 2016; EPUAP/NPIAP/PPPIA, 2019).
CHAIR-BOUND PATIENTS
A chair-bound patient must be repositioned as well. When a patient is seated, the weight of the body causes the greatest amount of pressure to occur over the ischial tuberosities. Since this area of the body is relatively small, the ischia bear intense pressure when a person is seated; without pressure relief, a pressure injury will occur quickly. If the patient cannot sit upright but slouches in the chair, then the sacral area is at risk as well. Pressure remains unrelieved in a paralyzed person because the small, involuntary movements that restore blood flow to the tissues are absent.
Specialized wheelchairs that offer a tilt and/or recline option may be indicated for positioning patients at risk of developing pressure injuries. Tilt and recline, though often confused, actually serve distinct and complementary positioning roles. Reclining a chair changes the hip angle and provides some pressure relief, but shearing forces may remain on the back. A tilt-in-space chair both tilts the head back and raises the feet up concurrently, thereby providing more pressure relief and less shearing forces.
Research has found that wheelchairs with tilt-in-space and recline mechanisms positively decrease sitting interface pressure and increase ischial blood flow. The bulk of the patient is moved from the seat of the wheelchair and is supported by the backrest. The degree to which this happens is proportionate to the tilt-and-recline angle of the wheelchair. Data suggest that even a small amount of tilt-and-recline angle can result in pressure relief to the tissues. However, meaningful increases in ischial bold flow were found only at greater angles of tilt-and-recline. At this time, there is no clear agreement on the period of time that tilt-and-recline should be done in order to effectively prevent pressure injury (Zemp et al., 2019).
General recommendations for the chair-bound patient include:
- Stand the patient and reseat them in the chair frequently, if possible.
- Provide adequate seat tilt to prevent sliding forward in the chair and adjust footrests and armrests to maintain proper posture and pressure redistribution.
- Elevate the legs or place the feet on a stool if the feet do not reach the floor in such a way as to slightly tilt the pelvis forward by positioning the thighs slightly lower than horizontally. This will prevent sliding forward out of the chair and reduce pressure on the sacrum.
- Elevate the feet and recline the chair by 30 degrees to reduce pressure.
- If the patient can change their own position, encourage pressure relief every 15 minutes. This includes chair pushups, leaning forward, leaning side to side, or tilting backwards. Leaning forward is the most effective and might be easier than chair push-ups.
- Acutely ill patients at risk for pressure injuries should not sit for longer than two hours at a time and not return to sitting for at least an hour.
- Patients who are incapable of changing their position while sitting should be repositioned at least every hour by a caregiver.
(EPUAP/NPIAP/PPPIA, 2019)
For a patient with an existing pressure injury:
- Minimize sitting time and consult a seating specialist if the injury worsens on the seating surface selected.
- Consider periods of bed rest to promote ischial and sacral pressure injury healing.
- Avoid sitting a patient with an ischial pressure injury in a fully erect posture.
- Patients with existing pressure injuries on the ischial areas should limit time sitting up in the chair to three times a day for 60 minutes or less, and they must use a cushion (gel or air cushions are best) that redistributes pressure.
(Bryant & Nix, 2016)
PHYSICAL AND OCCUPATIONAL THERAPY AND WHEELCHAIR POSITIONING
Physical and occupational therapists are of great importance in assessing and managing the immobile patient’s activities and instructing staff, patients, and families in proper techniques to prevent pressure injuries. This may include assessing the seating and positioning needs of individuals who are wheelchair bound. Proper wheelchair positioning with an individualized seating system can promote good posture, enhance breathing and digestion, prevent complications such as pressure injuries and skin irritation, slow further loss of mobility, minimize pain, and maximize functioning.
Components of a wheelchair seating system include appropriate size and width as well as specialized supportive cushions, backrests, headrests, and trunk, arm, and leg supports when indicated. The depth of the wheelchair, measured from back to front, must be adequate to provide support from the buttocks to the back of the knees. The floor-to-seat height, measured from floor to seating surface, must be sufficient to keep the patient’s thighs in a position parallel to the floor, with hip flexion as close to 90 degrees as possible (WOCN, 2016b).
PATIENTS WHO ARE UNABLE TO MAINTAIN REPOSITIONING
Some patients are unable to maintain position changes, such as patients with dementia or delirium. Since delirium diminishes a patient’s ability to recognize pressure and discomfort, it is recognized as a potential risk factor for pressure injury development. Approximately 5% of older individuals have some form of dementia (Eliopoulos, 2018). Delirium has been found to affect up to 56% of hospitalized older adults depending on the healthcare setting and pre-existing conditions (WOCN, 2016b).
Since delirium is reversible, every effort must be made to find the underlying cause, the most prevalent being:
- Pre-existing dementia
- Postoperative delirium
- Medications
- Dehydration
- Infection (e.g., urinary tract infection)
(Eliopoulos, 2018)
Each patient will have different risk factors for pressure injury, and each plan of care must be individualized. Pressure injury prevention for confused patients requires a holistic approach. Interventions include:
- Assessing whether the patient’s position looks comfortable:
- Is the patient’s shoulder jammed against the bed?
- Is the side-lying position more than 30 degrees?
- Is the sheet under the patient wrinkle-free and free from debris such as crumbs?
- Placing the patient in a quiet environment
- Minimizing bright lights
- Controlling the temperature
- Promoting rest and comfort (e.g., is the patient hungry, thirsty, in pain, or in need of toileting?)
(WOCN, 2016b; Eliopoulos, 2018)
PATIENTS WHO REFUSE CARE
Some patients may refuse care, refuse to be repositioned, refuse to use a pressure-relieving cushion in their chair, or refuse to participate in PT or OT. The first and most important action by the clinician is communication: Why is the patient refusing care?
- Is it related to their diagnosis, i.e., a traumatic injury such a spinal cord injury, a chronic condition such as rheumatoid arthritis, or a condition with an uncertain progression, such as multiple sclerosis?
- Is the patient exhibiting signs and symptoms of depression, such as irritability, fatigue, or hopelessness?
- Is a referral to a mental healthcare professional needed?
Open, honest communication with the patient, and if appropriate their caretakers, should address the importance of pressure injury prevention and the consequences of not implementing recommended interventions. When discussing potential complications of refusing care, clinicians must be candid and accurate in their descriptions of the complications so that the patient is left in no doubt about the seriousness of the decision they are making in refusing care and to protect the facility and clinicians against liability and future legal action.
Full, accurate, and objective documentation in the patient’s record is essential. The medical record must show:
- Education provided to the patient
- Frequency of patient education
- Consistent approach among clinicians
- Other interventions, such as involvement of the facility’s ethical committee
(Yankowsky, 2017)
It is the patient’s right to refuse care, but clinicians must ensure that facility policies and procedures are followed and that the patient is afforded every option to receive care.
Strategies clinicians can employ when treating patients who refuse care include:
- Empathize with the patient. Allow them to verbalize their feelings about their injury or condition. Remember that a loss of control in one’s life is frightening to everyone. Be a good listener.
- Avoid dictating and assuming control. Rather than telling the patient you are going to reposition them, ask them if they would be more comfortable if you helped them to change position.
- Look for the root cause of why the patient is refusing care. Remember that in the majority of cases there is a reason why the patient is not compliant with care.
- Ask the patient if there is anyone they would like to talk to, such as a close friend, a spiritual advisor, or someone who has had a similar traumatic injury.
- As a clinician, do not take the patient’s refusal of care personally. Do not allow personal emotions to interfere with patient interactions.
- Aim for small steps. If the patient will agree to a pressure-relieving cushion in a chair, it is a step in the right direction.
- Continue to educate the patient about why pressure relief is important.
- Remember that the patient is the primary member in the care team and continue to elicit their input on care.
- Remain friendly and caring in word and action; it is a known fact that patients cooperate more readily with clinicians they like.
(Collins, 2017)
CASE
Patricia is a 61-year-old female with multiple sclerosis, leaving her bedridden and unable to move her legs. Despite being on a pressure reduction surface, she has developed a stage 3 pressure injury at her sacrum because of refusing to be turned due to the severe pain she experiences from muscle spasms that are triggered each time her right leg is moved. This has made it very difficult for the staff to provide wound care and keep Patricia clean. Furthermore, pain medication has not been effective for Patricia’s very intense but brief episodes of pain.
The nurse asks the physical therapist for recommendations to make moving Patricia less painful for her and less stressful for the staff. After evaluating Patricia, the therapist recommends daily PT treatment, including localized heat treatments to her right leg and gentle active-assisted range of motion to her trunk and extremities prior to attempting bed mobility. PT sessions also focus on improving Patricia’s independence with functional bed mobility (as tolerated).
After several treatment sessions, Patricia is able to tolerate and actively assist with turning toward her right side and staying in position for the time needed to care for her wound and clean her. The therapist also instructs the staff about less painful ways to assist Patricia with bed mobility and positioning to allow wound care, in order to minimize discomfort to her lower extremities. As a result, Patricia is able to tolerate and even actively assist in turning from side to side, and her leg pain when repositioned is reduced to a more tolerable level.
Using Support Surfaces
Factors in the development of pressure injuries include prolonged pressure, friction/shear, and moist, warm skin. Each of these factors can be at least partially controlled by an appropriate surface for the bed and/or chair. A support surface is a specialized mattress or mattress overlay, chair cushion, or stretcher/operating room pad designed for the management of pressure loads and microclimate. (Microclimate is the term used to describe the local tissue temperature and moisture at the body/support interface, and microclimate control is a function of some support surfaces.) (See also “Emerging Therapies” later in this course.)
Pressure redistribution is the most important feature of a support surface. The body’s tissues can withstand higher loads of pressure for short periods of time and lower loads for longer periods of time. A surface that effectively redistributes pressure across the entire body (contact) surface effectively reduces the amount of pressure and extends the time a patient can safely remain in one position (WOCN, 2016b; EPUAP/NPIAP/PPPIA, 2019).
It is critical to remember, however, that there is no mattress, cushion, or bed available today, at any price, that will eliminate pressure and relieve the clinician or caregiver from having to reposition the patient. Patients must still be repositioned no matter what surface is used. Likewise, pressure is not the only contributing factor to skin breakdown and does not replace attention to perfusion, nutritional support, and management of comorbidities (WOCN, 2016b).
IMMERSION, ENVELOPMENT, AND BOTTOMING OUT
In order to redistribute pressure, a support surface must conform to the contours of the body through immersion and envelopment. Immersion is the depth to which the body “sinks into” the surface. As the body does this, the pressure is spread out along the body surface. Immersion is dependent on the stiffness and thickness of the support surface and the flexibility of its cover.
Envelopment is the ability of the support surface to conform to irregularities such as clothing, bedding, and bony prominences without causing substantial increase in pressure. This maximizes pressure redistribution.
In contrast to the functions of immersion and envelopment, the term bottoming out is used to indicate excessive penetration of the surface, meaning the body sinks so deeply into the surface that its bony prominences are actually resting on the underlying bed frame. Factors that contribute to bottoming out include:
- Patient weight that exceeds the support surface’s limits
- A disproportion between weight and size, such as in a patient with bilateral leg amputations, which results in more of the body weight being concentrated in the trunk
- Consistently keeping the head of the bed over 30 degrees
- Inadequate support settings such as under- or overinflation
For some support surfaces, bottoming out can be evaluated by placing one’s hand palm-up beneath the support surface in the area underlying the patient’s bony prominence. If the patient’s bony prominence can be felt by the hand, then the support surface is not supporting the patient properly. However, many support surfaces cannot be assessed this way; the clinician must contact the equipment department of the facility or the supplier or manufacturer of the support surface for information on how to assess the functioning of the support surface.
COMPONENTS OF A SUPPORT SURFACE
The most important component of a support surface is the medium used to provide the pressure redistribution. This can be air, fluid, or solid, alone or in combination.
Foam is a solid material and is available in all configurations. Foam surfaces are generally low-cost and lightweight and require minimal maintenance. Disadvantages include the fact that foam does not last long since it compresses over time; it absorbs moisture (which can be a potential for infection); and it is hard to dispose of. Closed-cell foam does not allow air through, which can increase skin temperature, while open-cell foam does allow air to enter and exit, making it more conformable to the body. One type of open-cell foam is memory foam. If a foam pad is used on top of a mattress (known as an overlay) to redistribute pressure, it needs to be at least three inches thick.
Gel pads contain a mix of substances that allow them to respond like memory foam. They are good at preventing shear, but they can result in increased skin moisture.
Fluid support surfaces include a viscous substance that is thick but free-flowing, which allows it to redistribute weight. Water-filled surfaces reduce pressure better than a standard mattress but are undesirable for use in a hospital due to multiple concerns, such as temperature control, leakage, difficulty with transfers, performance of CPR, and the time and labor involved in draining the mattress and moving the bed.
Air is frequently used in support surfaces; however air-filled surfaces have the potential to leak if damaged and require either periodic manual reinflation (if nonpowered) or an electric pump to remain inflated. Studies show that low-air-loss surfaces prevent the accumulation of moisture and resultant skin maceration (Baranoski & Ayello, 2016; EPUAP/NPIAP/PPPIA, 2019).
Some support surfaces have low-friction covers (like Gore-Tex) to reduce friction so that the skin slides more easily over the surface without putting strain on the skin that could cause damage. However, even these support surfaces cannot provide total prevention against the shearing that occurs when the patient slides down in bed when the head is raised; other interventions are needed to prevent that (WOCN, 2016b).
CATEGORIES OF SUPPORT SURFACES
Support surfaces are commonly used in a variety of applications:
- Mattresses and mattress overlays
- Operating room bed surfaces
- Examination and procedure table surfaces
- Pads for emergency and transport stretchers or gurneys
General categories of support surfaces include mattresses, overlays, and integrated bed systems. Specific features include cushions and pads. They may be powered or nonpowered, active or reactive. Added features may include low air-loss, air-fluidization, lateral rotation, and alternating pressure (see below).
Rings, foam cutouts, or donuts under the patient should not be used as support surfaces, as these concentrate pressure on surrounding tissue, causing swelling and decreasing circulation. The fact that they can be found in medical supply stores does not mean they are safe to use.
With the use of any support surface, the number of linens and other items used under the patient must be kept at a minimum or the pressure-reducing ability of the surface will be altered significantly. Staff, patients, and family members must be instructed to use no more than two items between the patient and the surface (e.g., one pull sheet and one incontinence pad or product).
General Categories
Mattresses can be composed of any medium or a combination, and may require a specialized bed frame. They create much less risk of bottoming out and can provide other therapeutic functions such as reduced friction and shear and improved microclimate management between the patient’s skin and the surface.
Overlays can be composed of any medium and are placed on top of an existing mattress. They are thinner than mattresses, putting the patient at risk for bottoming out. Other drawbacks are: they elevate the height of the sleep surface, can complicate patient transfers, alter the fit of linens, and increase the risk of falls or entrapments. When a foam overlay is used, it should be a minimum of three inches thick to provide pressure redistribution.
Integrated bed systems are comprised of the support surface and bed frame combined into a single unit. Their advantage is that the frame may include many features to make the bed easier and safer to use, such as alarms, scales, and the ability to support more weight.
Specific Categories
Procedure, transport, ER, and OR mattresses are used for patients who need a support surface in bed, since this means they also need one while on gurneys or tables. Many companies provide pressure redistribution pads for surfaces other than beds.
Chair cushions are utilized for patients who sit for a long time in order to reduce the risk for ischial pressure injuries. These cushions must be matched to the patient based on size, posture, mobility, and lifestyle needs, and include covers that can dissipate heat. Some specialized wheelchair cushions may also address incontinence.
Active surfaces can be either a powered mattress or an overlay that changes its load distribution whether or not someone is on the surface (called alternating pressure). The air cells in such surfaces cyclically inflate and deflate, which changes the areas of the body under pressure. These are recommended for patients at high risk and for whom frequent manual repositioning is not possible.
Reactive surfaces move only in response to the patient’s body. These can be powered or nonpowered (nonpowered also being referred to as static air surfaces). These are low-tech, compact, and low in weight (Edsberg et al., 2016). They are available as chair cushions, overlays, mattresses, and procedure pads. All reactive support surfaces are appropriate for pressure injury prevention in patients who are frequently repositioned. Some are appropriate for patients with existing pressure injuries.
Low-air-loss surfaces have a pump that provides a slow, continuous airflow into the mattress for even pressure distribution and continuous airflow across the skin for microclimate management. The amount of pressure in the mattress can be adjusted for the height and weight of the patient, and the mattress further adjusts when a patient sits up in bed to prevent bottoming out. Controls allow instant deflation for CPR. They cannot be used on patients with unstable spines.
Air-fluidized surfaces contain silicone-coated beads that provide both air and fluid support. When air is pumped through the beads, the beads behave like a liquid and the patient floats, with two thirds of the body immersed in the warm, dry beads. When the bed is turned off, it becomes hard enough for repositioning or CPR. Some beds now combine air-fluidized therapy in the lower half of the bed and low air-loss in the upper half, allowing the bed to be adjustable. This is a very expensive therapy and should only be used for patients who require very high-level care, such as those with multiple wounds or flap procedures (a surgical procedure to close a pressure injury). The beds are also extremely heavy and may not be safe in a home.
Lateral rotation is used to prevent and treat certain cardiopulmonary conditions. With this feature, the patient is continually rotated from side to side. While some low-air-loss beds may incorporate lateral rotation, this does not eliminate the need for routine manual repositioning. This is because when the bed turns the patient, the patient’s skin and tissues never leave the surface of the bed, and thus pressure is not relieved (WOCN, 2016b).
CHOOSING A SURFACE
A support surface must be selected to will meet the patient’s needs for pressure redistribution based on the following factors:
- Level of immobility and inactivity
- Need for microclimate control and shear reduction
- Size and weight of the patient
- Risk for development of new pressure injuries
- Number, severity, and location of existing pressure injuries
(Bryant & Nix, 2016; EPUAP/NPIAP/PPPIA, 2019)
Other factors to consider include:
- Fall and entrapment risk (overlays and mattresses can increase the height of the sleep surface)
- In a patient who is a candidate for progressive mobility, a surface that makes it easier to get out of bed
- Compatibility of the surface with the care setting
- Availability of the product
- Previous support surface usage and patient preference
- Achievement of specific outcomes (i.e., prevention of pressure injury)
(WOCN, 2016b; Bryant & Nix, 2016; EPUAP/NPIAP/PPPIA, 2019)
Determining the appropriate support surface is based first on the patient’s condition and the healthcare setting. Overall, if the patient is able to be turned and has at least two intact turning surfaces, meaning the skin is intact on two sides of the body (e.g., the right and left trochanters), then a mattress overlay or an alternating pressure pad can be used over a regular mattress. If the patient has skin breakdown on more than one side of the body, then a mattress replacement should be used. Depending on the healthcare setting, patients who already have stage 3 or 4 pressure injuries on their trunks qualify for a mattress replacement.
Cost and product availability are secondary considerations in choosing a surface. The healthcare setting will also determine the product used. For instance, in the home setting the weight of the bed, the structure of the home, the width of the doors, and the availability of uninterrupted electrical power will have a major impact on the support surface available for use. A patient’s health insurance may be a significant determining factor as to which surface will be available to the patient.
In general, a standard hospital mattress should not be used with at-risk patients. It is important to contact the medical equipment department to determine what is available for pressure reduction (WOCN, 2016a).
Patient Size and Weight
The support surface chosen must be approved for the patient’s body size and weight. Most conventional support surfaces are for patients who weigh 300 pounds or less. If the patient weighs more than this, then a bariatric mattress and frame must be obtained.
Even in patients who weigh less than the weight limit, where their weight is concentrated may make a difference in the mattress needed. The mattress may not be able to support the patient when the body weight is not evenly distributed. For instance, a paralyzed patient or an amputee may weigh under the limit, but most of the weight will be concentrated in the trunk. If it looks as though the patient is lying or sitting in a “well,” the surface may not be able to support the patient’s weight.
In the event a surface does not appear to be supporting a patient’s weight—and provided the support surface is the correct one—it is important to check for any disconnected hoses or improper machine settings. It may also be necessary to contact the appropriate hospital department, supplier, or manufacturer to have the support surface checked as needed. It is also important to ensure that all staff caring for the patient are aware of the features of the support system (EPUAP/NPIAP/PPPIA, 2019).
Managing Moisture
Moisture can lead to skin damage of various types. Incontinence-associated dermatitis (IAD) is the most common form of moisture-associated skin damage and is frequently misidentified as a pressure injury. While they are not the same thing, preventing IAD can also help to prevent the formation of pressure injuries.
TYPES OF SKIN DAMAGE DUE TO MOISTURE
Moisture-associated skin damage (MASD) is defined as inflammation and erosion of skin caused by prolonged exposure to various sources of moisture, including urine or stool, perspiration, wound exudate, mucus, or saliva. The four forms of MASD are:
- Incontinence-associated dermatitis (IAD)
- Intertriginous dermatitis (ITD)
- Periwound moisture-associated skin damage
- Peristomal moisture-associated skin damage
(WOCN, 2016b; EPUAP/NPIAP/PPPIA, 2019)
Incontinence-associated dermatitis due to urinary incontinence may involve the perineum and the area between the vulva and scrotum or anus. IAD due to fecal incontinence may involve the anus, buttocks, coccyx, perigenital areas, groin folds, and posterior thigh regions. Its characteristics are moist, bright-red skin, inflammation, denudement (skin stripped raw), erosion, and blisters. The damage is usually superficial but can progress to full-thickness lesions. The patient will complain of burning, pain, and itching.
Moisture alone causes maceration, but acute inflammation and skin loss are due to a combination of maceration and some other source of injury such as a chemical irritant, friction, or pathogenic invasion. Wet skin loses strength and is more prone to damage from friction and shearing. It allows irritants to penetrate the epidermal layers of skin, which then allows common pathogens such as Candida and Staphylococcus to enter (WOCN, 2016b).
Skin injury by friction appears as redness and progresses to abrasion. It occurs when skin is rubbed vigorously during cleaning or when skin rubs against incontinence garments or bed or chair surfaces. Areas of skin rubbing against each other cause “kissing” lesions such as are seen between the buttocks cheeks.
Mechanical damage (friction) abrades and disrupts the skin from the “top down,” whereas pressure and shear cause blood vessel compression and ischemic damage from the “bottom up.” Determining the cause of the lesion—and distinguishing between IAD and a pressure injury—includes an assessment of the location, characteristics, and most importantly, the patient’s history.
| Friction (top down) |
IAD (top down) |
Pressure/Shear (bottom up) |
|
|---|---|---|---|
| (WOCN, 2016b) | |||
| Location | Fleshy surfaces exposed to repetitive rubbing | Perineal area, inner thighs, buttocks | Bony prominences, under medical devices |
| Depth | Superficial | Superficial | Full thickness |
| Characteristics | Pink/red wounds without necrosis | Edges indistinct, fungal rashes common, pink/red wounds without necrosis | Well-defined lesions, tunneling and undermining, tissue necrosis |
| History | Restlessness, frequent sliding, malnourished, diaphoretic, on steroids | Prolonged or recurrent exposure to urine and/or stool | Prolonged immobility, sliding, use of medical device at site of damage |
MANAGING INCONTINENCE
It is important to cleanse skin gently with a pH-balanced cleanser at each incidence of soiling. Perineal skin cleansers are more effective for prevention and treatment of IAD than traditional soap and water. This is because bar soap, which is alkaline and very drying, disrupts the skin’s protective abilities. Vigorous cleaning, as well as the use of rough washcloths, can also lead to skin erosion. Soft, disposable cloths are easier on the skin. Fragrance or alcohol are irritants, and cleaning products containing these are to be avoided. Some facilities use no-rinse foams, which are another good option.
An incontinence skin barrier product should be used to protect the skin after cleansing. Products such as creams, ointments, pastes, or those that form a film on the skin are all useful. Protective products with dimethicone, petroleum, or zinc oxide are recommended for patients with fecal incontinence or both urinary and fecal incontinence to protect against IAD. Several manufacturers offer products that both clean and protect, saving time for the caregiver and increasing the likelihood that perineal care will be performed.
Absorbent underpads or incontinence briefs are chosen to wick moisture away from the skin instead of trapping the moisture against the skin. However, all briefs increase moisture at the perineal region because they are occlusive and do not “breathe.” This creates warmth near the skin that, when combined with moisture, ammonia, and enzymes, increases skin breakdown. There is an increased risk with the use of briefs because they may not be changed as often as they should be due to the difficulty in seeing when a patient has voided. Briefs are not recommended for fecal incontinence because they can trap stool against the skin.
Many hospitals have moved away from using briefs except when a patient is ambulating or going off the unit. Instead, they use underpads that are especially designed to keep the skin dry and breathable and do not allow heat or moisture to be trapped against the skin.
A toileting program can also decrease incontinence and thus IAD. In situations where the severity of urinary incontinence has contributed to or may contaminate an existing pressure injury, placing a urinary catheter may be indicated (WOCN, 2016a).
Much attention has been paid to infections related to the use of indwelling catheters, particularly since 2008, when the Center for Medicare and Medicaid Services changed reimbursement regulations, calling catheter-associated urinary tract infections (CAUTI) “preventable harm” and withholding payment for additional costs related to CAUTI treatment (WOCN, 2016c). Significant bacterial colonization occurs within a few days of catheter insertion, which can lead to infection. The prevention of CAUTI begins with the decision to not insert a catheter.
The CDC has developed guidelines for the appropriate use of indwelling catheters as follows:
- To manage urinary retention or bladder outlet obstruction
- To provide accurate urine output measurements
- To manage bladder short term following select surgical procedures
- To assist in the healing of perineal wounds at risk of contamination by urine
- To improve comfort at end of life
(WOCN, 2016c)
Therefore, incontinence is not a valid reason for insertion of an indwelling catheter to replace alternative means of care for the incontinent patient. It can be used in the treatment of a wound but not in prevention, since the risk of CAUTI is too high (WOCN, 2016c).
| Type | Description | Causes/Associated Factors |
|---|---|---|
| (WOCN, 2016c) | ||
| Urge incontinence | Involuntary loss of urine with an abrupt strong need to void; occurs with the involuntary contractions of the detrusor muscle or uncontrolled urethral relaxation | Associated neurological disorders include stroke, paraplegia, multiple sclerosis, Parkinsonism, or dementia. |
| Stress incontinence | Involuntary leakage of small amounts of urine with a rise in intra-abdominal pressure that occurs during coughing, sneezing, laughing, and physical activity | Often seen in women; causes include estrogen deficiency, weakness in pelvic floor musculature, urethral sphincter weakness, childbirth, and obesity. |
| Functional incontinence | Having a functional urinary tract but unable or unwilling to get to the toilet to urinate | Often occurs in older adults; contributing factors include use of physical restraints, musculoskeletal dysfunction, unavailability of a urinal, visual impairment, impaired mobility, cognitive deficits, unfamiliarity of environment, and psychosocial difficulties. |
| Overflow incontinence | Involuntary loss of urine secondary to overdistension of the bladder; results in the leakage of small amounts of urine due to an outflow obstruction or a hypotonic bladder | Common causes include medications, neurological conditions such as diabetic neuropathy or spinal cord injury, prostate enlargement, detrusor weakness, or urethra stricture. |
| Mixed incontinence | Combination of other types of urinary incontinence, typically urge and stress incontinence | Common in older adults. |
OCCUPATIONAL AND PHYSICAL THERAPY AND INCONTINENCE
Occupational and physical therapists are both specialists in assessing, identifying, and treating the underlying impairments associated with urinary incontinence. Common interventions that can be implemented by these professionals may include:
- Pelvic floor muscle training (PFMT): a program of repeated pelvic floor muscle contractions, which involves specific and progressive learned exercises to consciously contract the pelvic floor muscles, found to be useful in preventing urinary incontinence, overactive bladder, and postvoid dribbling
- Scheduled toileting (i.e., timed voiding): monitoring and then matching of the individual’s typical toileting schedule
- Habit retraining: identifying the individual’s natural voiding pattern and developing an individualized toileting schedule
- Prompted voiding: establishing a routine in which a caregiver suggests voiding and provides assistance as needed
- Biofeedback: using an external sensor placed in close proximity to the anal orifice to detect contraction of the pelvic floor muscles in order to help the patient to identify and strengthen those muscles
- Electrical stimulation: using electrodes placed in either the vagina or rectum to stimulate and strengthen pelvic floor muscles, thereby aiding pelvic floor muscle contractions
Research indicates that the use of a toileting routine in combination with medication and education results in decreasing urinary incontinence.
(APTA, 2016; Healthline, 2016; NAFC, 2018; Vasavada, 2019; WOCN, 2016c)
TREATING FECAL INCONTINENCE
Fecal incontinence occurs when structures controlling defecation do not function correctly, usually because of diarrhea, trauma to the structures, or nerve damage.
- Causes of diarrhea include anything that increases gut motility or decreases water absorption, including medications, certain foods, and diseases that cause intestinal inflammation.
- Trauma to the structures includes scarring from chronic inflammation (as in irritable bowel syndrome), radiation, surgery, and childbirth.
- Nerve damage can also be the result of childbirth or of spinal cord injury, multiple sclerosis, Parkinson’s disease, stroke, and diabetic neuropathy.
Those with cognitive difficulties may not perceive the need to defecate. Patients with fecal incontinence should be referred to a specialist for accurate diagnosis and appropriate treatment.
When the underlying cause cannot be treated, regulation of bowel function by promoting ideal stool consistency can lead to few or no periods of incontinence. Modifying the diet can help, as certain foods can exacerbate fecal incontinence, such as alcohol, caffeine, fruit, gas-producing foods, sugar-free products that contain sorbitol, and dairy products for those who are lactose-intolerant. Dietary fiber adds bulk and can improve passage of stool.
Adequate fluid intake is essential because dietary fiber pulls water into the feces; without adequate water the patient will have very dry stools that are difficult to pass.
Emptying the bowel at regular intervals through time-toileting, digital stimulation, or use of suppositories prevents incontinence because an empty rectum will not leak.
Incontinence containment products are useful in community settings, but a plan for skin protection must be in place. In hospital settings, fecal management systems can be used. A colostomy is also an option if everything else has failed and quality of life is severely restricted due to fecal incontinence (Gump & Schmelzer, 2016).
CASE
Ruth is an elderly woman living in a residential treatment facility. She ambulates with assistance, and requires hands-on assistance with toileting and self care. She has a stage 3 pressure injury on her sacrum that the nurse is treating per physician’s orders. The home health nurse has been educating the facility’s caregivers about the importance of keeping Ruth’s perineal skin clean, dry, and protected.
The nurse knows that exposure to urine can delay or prevent wound healing. Remembering that frequent dressing changes can also delay healing, the nurse advises the physician of Ruth’s incontinence and wound status. The nurse also asks the physician for referrals to physical therapy and occupational therapy in order to further evaluate Ruth.
After completing an initial evaluation, the physical therapist believes that Ruth would benefit from gait training with a front-wheeled walker in order to improve her ambulation safety. The occupational therapist also evaluates the patient and recommends a timed voiding program along with verbal voiding prompts, a raised toilet seat, and grab bars in the bathroom; he believes that Ruth’s mild cognitive decline would not make her a good candidate for biofeedback.
At the end of four weeks of following the timed voiding schedule, the nurse compares the wound’s condition and measurements and finds that there is now granulation tissue in the wound bed and that the wound size has decreased by 75%. The nurse and occupational therapist recommend long-term continuation of the individualized toileting regime to maintain continence and prevent further pressure injury.
Managing Nutrition
Malnutrition is associated with overall morbidity and mortality. Assessing the patient’s nutritional status must be part of the total assessment for pressure injury risk. A nutrition assessment should be performed upon admission and whenever there is a change in the patient’s condition that puts them at risk for malnutrition.
Malnutrition places patients at greater risk for developing pressure injury. Malnutrition is defined as the presence of two or more of the following characteristics:
- Unintended weight loss
- Loss of muscle mass
- Loss of subcutaneous tissue
- Localized or generalized fluid accumulation
- Decreased functional status
A low body mass index (BMI) is a factor related to pressure injury development. With a low BMI due to poor nutritional intake, there is a diminished quantity of subcutaneous tissue and decreased protection of the skin. In studies conducted with ICU patients in the United States and in hospitalized patients in Australia, the prevalence of pressure injury was greatest among patients who were underweight or very obese (Efraim, 2018).
NUTRITION ASSESSMENT PARAMETERS
- Current weight and usual weight
- History of unintentional weight loss or gain (>5% change in 30 days or >10% change in 180 days)
- Body mass index (BMI)
- Food intake
- Dental health
- Ability to chew, swallow, and feed oneself
- Medical and/or surgical history that influences intake or absorption of nutrients
- Drug-food interactions
- Psychosocial factors that can affect food intake
- Ability to obtain and pay for food
- Facilities for cooking and eating
- Food preferences
- Cultural and lifestyle influences on food selection
- Over 65 years of age
The patient should be monitored for signs of dehydration, such as decreased skin turgor and/or urine output or elevated serum sodium. Serum protein tests, such as for albumin and pre-albumin, may be affected by inflammation, renal function, and hydration and so may not correspond with overall nutritional status. Thus, laboratory tests should be considered as only one part of the nutritional assessment.
Recent weight loss in older adults is a key factor in mortality risk. The “anorexia of aging”—which includes appetite decline, weight loss, and decreased metabolic rate—places the older adult at risk for malnutrition. While unintended weight loss is a risk factor for malnutrition, bariatric adults may also be poorly nourished (Bryant & Nix, 2016).
Following are dietary recommendations for those who are at risk or have an existing pressure injury and who are at risk for malnutrition:
- Calorie intake of 30 kcal to 35 kcal per kg of body weight
- Protein intake of 1.25 g to 1.5 g protein per kg of body weight
- Supplementation with high-calorie, high-protein, arginine (an amino acid), and vitamins and minerals when nutritional needs cannot be met with dietary intake
- Adequate daily fluid intake
Renal function is also assessed to ensure that high levels of protein are appropriate for the patient (Baranoski & Ayello, 2016; EPUAP/NPIAP/PPPIA, 2019).
Any patient with nutritional and pressure injury risks, suspected or identified nutritional deficiencies, or a need for nutritional supplementation to prevent undernutrition should be referred to a registered dietitian. Any patient with a pressure injury should be referred to the dietitian as well (WOCN, 2016a).
Emerging Therapies for Pressure Injury Prevention
Emerging therapies for pressure injury prevention include microclimate manipulation, fabrics designed to reduce shear and friction, and use of prophylactic dressings (WOCN, 2016a).
MICROCLIMATE CONTROL
Microclimate is the term used to describe the local tissue temperature and moisture at the body/support interface, and microclimate control is a function of some support surfaces. This feature can be of benefit to patients who are diaphoretic (sweat heavily) or with elevated temperatures and perspiration, since they are at increased risk for developing pressure injuries. For instance, elderly patients have a reduced ability to dissipate excess heat, resulting in skin warming. High levels of moisture from perspiration, incontinence, or drainage result in maceration, which reduces skin strength and increases damage caused by friction (WOCN, 2016b; Bryant & Nix, 2016; EPUAP/NPIAP/PPPIA, 2019).
The need for moisture and temperature control should be considered when selecting a support surface. A support surface with microclimate control can help maintain normal skin hydration and temperature through the use of porous covers that promote air transfer between the skin and surface, which results in the decrease of moisture and body heat. Other surfaces pump air through microperforations in the support cover to decrease moisture and heat (WOCN, 2016a).
FABRICS
Silk-like fabrics rather than cotton or cotton-blend fabrics can be used to reduce friction and shear. Research has shown that the use of silk-like fabric undergarments, booties, and linen (alone or in combination) significantly reduces the incidence of pressure injury development and reduces the deterioration of existing pressure injuries (Freeman, 2017; EPUAP/NPIAP/PPPIA, 2019).
PROPHYLACTIC DRESSINGS
A polyurethane foam dressing can be applied prophylactically to bony prominences (e.g., heels, sacrum) to reduce friction, shearing, and moisture damage and thereby help prevent pressure injuries in anatomical areas frequently subjected to friction and shear. Trials have indicated that the application of specialty foam dressings to the sacrum is effective in reducing the rate of pressure injury in ICU patients and in nursing home residents who are at high risk for pressure injury development. Research also indicates that the application of multilayer foam dressings to the sacrum of patients before undergoing cardiac surgery greatly reduces the incidence of pressure injury in the immediate postoperative period (first five days in the ICU and progressive care units) (Strauss et al., 2019; EPUAP/NPIAP/PPPIA, 2019).
Considerations when selecting a prophylactic dressing include:
- Ability of the dressing to manage microclimate
- Ease of application and removal
- Ability to regularly assess the skin
- Anatomical location where the dressing will be applied
- The correct dressing size based on area to be protected
Foam dressings have a greater ability to absorb moisture than film or hydrocolloids and often have easy-to-lift borders. They are also permeable to water vapor and gases. Some dressings adhere well but can damage fragile skin on removal. All other preventive measures must be continued along with the dressings; the skin must still be inspected daily and the dressings replaced as needed (Ayello & Baranoski, 2016; EPUAP/NPIAP/PPPIA, 2019).
Preventing Pressure Injury in Special Populations
PATIENTS WITH MEDICAL DEVICES
With the recognition that the use of medical devices can contribute to pressure injury formation, NPIAP has also developed “Best Practices for Prevention of Medical Device-Related Pressure Injuries (MDRPI)” (NPIAP, 2016b; EPUAP/NPIAP/PPPIA, 2019). These include:
- Choose the correct size of medical devices to fit the individual.
- Cushion and protect the skin with dressings in high-risk areas (e.g., nasal bridge).
- Remove or move the device daily to assess skin.
- Avoid placement of devices over sites of prior or existing pressure injury.
- Educate staff (and caregivers) on correct use of devices and prevention of pressure injury.
- Be aware of edema under devices and potential for pressure injury.
- Confirm that devices are not placed directly under an individual who is bedridden or immobile.
- Ensure that all members of the patient care team, particularly respiratory therapy, are involved in the plan for reduction of MDRPI.
(Camacho-Del Rio, 2018)
BARIATRIC PATIENTS
Pressure injury prevention and treatment for bariatric patients is similar to that for nonbariatric patients; however, it is also more challenging for a number of reasons:
- The bariatric patient has increased difficulty moving, either independently or with assistance.
- Increased body weight makes it difficult to view bony prominences and to redistribute pressure.
- Shear and friction are often increased, as the patient is inclined to drag the heels and sacrum when getting out of bed.
- The increased pressure on the bowel and bladder from abdominal weight increases the risk of stress incontinence and diaphoresis, which increases the risk of skin maceration.
- Obesity can compromise respiration due to impaired diaphragmatic movement and lead to subsequent impaired tissue perfusion.
- Pressure injuries develop over bony prominences but may also result from tissue pressure across the buttocks and other areas of high adipose tissue concentration. They may develop in unique locations, such as underneath folds of skin and in locations where devices may have been compressed between skin folds.
- The weight of the pannus (the skin “apron”) can cause pressure injuries to develop in areas such as the hip, thighs, trunk, and torso.
- Skin must be checked for maceration, which is common due to increased diaphoresis.
- Additional positioning devices may be needed to offload the pannus or other large skin folds.
- Infection and delayed healing are more common.
- Deeper tissue layers can impede assessment of cavity wounds and increase the risk of retained wound dressings.
- Equipment must be provided that is the appropriate size and great care taken that neither the patient nor the staff are injured during the provision of care.
(Bryant & Nix, 2016; EPUAP/NPIAP/PPPIA, 2019)
INTERTRIGINOUS DERMATITIS
It is important that the clinician recognize the difference between intertriginous dermatitis (intertrigo) and stage 1 and 2 pressure injuries. Intertrigo is an inflammatory skin condition that affects opposing skin surfaces, caused by trapped moisture and friction between the opposing skin folds (i.e., skin rubbing against skin) (WOCN, 2016b).
Intertrigo can progress to severe inflammation with mirrored areas of skin erosion or even ulceration. Linear skin tears at the base of the skin fold occur when the skin is pulled or stretched when skin folds are separated, such as occurs during cleaning. Complications include secondary infections such as candidiasis and bacterial infections. These erosions and skin tears are not pressure injuries.
Bariatric patients are at high risk for this dermatitis because their multiple skin folds form ideal conditions for inflammation and maceration. The differentiation on whether the lesion is intertrigo or a pressure injury is based on the etiology of the skin damage and the appearance (see the definitions of stage 1 and 2 pressure injuries later in this course). The most common areas for intertrigo to develop are under the pannus, the breasts, between the buttock cheeks, and in the groin or perineum.
PEDIATRIC PATIENTS
There is growing awareness that pressure injuries can be the basis of illness, suffering, and increased cost of care in the pediatric population. A study assessing neonatal ICU unit patients found that almost 80% of pressure injury present was device related, and over 90% of MDRPI developed in premature infants. Statistics demonstrate little change in the incidence of pediatric pressure injuries since 2010 (Delmore et al., 2019).
Pressure injuries in children cannot be presumed to be uncommon, and a pressure injury risk assessment is as important in this population as it is in adults. There are pressure injury risk assessment tools for pediatrics. Two of them are the Braden Q and the Pediatric Pressure Ulcer Prediction and Evaluation Tool (PPUPET).
The most recently developed instrument for measuring pressure injury in the pediatric population, the Braden QD, was presented in 2018. It is based on the original Braden Q scale and intended for use in neonates to patients 21 years of age. The Braden QD scale incorporates the five subsets of the Braden Q scale along with the inclusion of two new subsets: the number of medical devices in use and patient repositionability/skin protection (Curley et al., 2018).
Several factors are associated with pediatric pressure injury development:
- Low birth weight
- Skin texture (e.g., neonatal skin is very thin)
- Incubator temperature and humidity
- Support surface used
- Limited position changes
- Endotracheal intubation
- Incontinence
- Poor tissue perfusion
- Fever
- Larger head proportion to the body, putting the occiput at high risk for pressure injury development
Consider children with medical devices to be at greater risk for pressure injuries. At particularly high risk are those with mechanical ventilation, including tracheostomies, CPAP or BPAP, and ECMO. One study found that 35% of pressure injuries resulted from tracheostomy fixation devices (Delmore et al., 2019). Pressure injury at the tracheostomy site can be due to the fact that the device rests directly on the patient’s skin. The pressure injury can occur directly under the tracheostomy tube or at different location under the ties used to secure the tracheostomy tube in place (Odom et al., 2020).
Increased temperatures, moisture, and humidity under medical devices and their securement can greatly increase the risk for pressure injury in pediatric patients. Proactive, preventive care should be the primary goal for clinicians, and the use of absorptive dressings under medical devices should be used whenever feasible (Boyar, 2019b).
Many pediatric patients with medical device–related pressure injury are younger, with premature infants being particularly vulnerable. One of the major reasons for this vulnerability is immature skin, with neonates and infants under 2 years of age at the highest risk level.
Neonates have a much thinner stratum corneum, which is the outermost layer of the epidermis, compared to full-term infants. For neonates less than 24 weeks of gestational age, the stratum corneum maybe almost completely absent. Another factor that predisposes the premature skin of pediatric patients to pressure injury is the reduced interconnection between the epidermal and dermal layers of the skin. This places the premature skin of neonates at greater risk for damage associated with friction (Delmore et al., 2019).
There is limited information available on healing times for pressure injuries in the pediatric population. One small study that included pediatric patients with pressure injuries at stages 2 to 4 demonstrated an average healing time of 13 days. However, more detailed research needs to be done in this area, taking into consideration the gestational age of the infants and comorbidities. A retrospective study done at Arkansas Children’s Hospital found that the use of a foam dressing and wound filler silver product during the first 14 days of treatment assisted with healing of tracheostomy-related pressure injuries (Odom et al., 2020).
Immobility-related pressure injury is another major area of concern in the pediatric population. The occipital region is the area most often affected by immobility-related injuries especially in infants from birth to three years of age. In infants the head encompasses a higher percentage of body weight and surface area, and when the pediatric patient is lying supine, the occipital area is the main pressure point and at substantial risk for pressure injury (Bryant & Ayello, 2016).
As in adults, assessment and monitoring, involvement of the family, nutritional management, support surfaces, and repositioning are important. Wound care strategies and dressing selections must be taken with great care, as baby skin is more permeable and more fragile than adult skin, with the result that products commonly used on adults may not be appropriate for children, such as skin preps, barrier products, antimicrobials, and adhesives. Wound care product choices should be discussed with pediatric specialists (EPUAP/NPIAP/PPPIA, 2019).
SPINAL CORD INJURY PATIENTS
The development of pressure injury is of special concern to individuals with spinal cord injury. Pressure injury is the second most frequently occurring medical complication among those with spinal cord injury. Data demonstrate that >95% of adults with spinal cord injury will develop one or more pressure injuries during their lives. Lack of mobility and paralysis is a key factor in pressure injury occurrence; the greater the level of paralysis, the greater the risk for the development of pressure injury.
In a study of community-dwelling individuals with spinal cord injury, it was found that those with spinal cord injury at the cervical level had a higher risk of developing a pressure injury compared to those with a spinal cord injury at the lumbar level (Cowan et al., 2019).
In another study of individuals with spinal cord injury living in long-term care facilities, researchers found a higher incidence of pressure injury in patients who were paraplegic than those who were tetraplegic. This may be because patients who are tetraplegic require total care from the facility staff, whereas patients who are paraplegic have more responsibility for making position shifts aimed at relieving pressure, especially when sitting. Another finding was a greater risk for malnutrition in patients with paraplegia compared to those with quadriplegia, perhaps due to a greater calorie use in paraplegic patients due to upper body mobility and potential unaddressed difficulties with independent feeding in this group.
Recommendations include the implementation of greater preventive measures among long-term care patients who are paraplegic to prevent pressure injury. Specific suggestions included closer and more consistent monitoring of this high-risk population, better utilization of assistive technology, and increased patient motivation and education regarding pressure injury prevention (Cowan et al., 2019).