EPIDEMIOLOGY
Incidence and Mortality
The third most common cancer in the United States is lung cancer, according to recent statistics from the Centers for Disease Control and Prevention (CDC). The most common form of cancer is skin cancer. Breast cancer (among women) and prostate cancer (among men) are the next most common cancers in the United States. Lung cancer has the highest mortality among cancers in the United States, regardless of gender (CDC, 2021c). The greatest risk of lung cancer is from smoking, though lung cancer can occur in people who have never smoked.
Lung cancer incidence has been declining since the mid-1980s in men but only since the mid-2000s in women because of gender differences in historical patterns of smoking uptake and cessation. Since the mid-2000s, incidence has decreased steadily by about 2% per year overall but at a faster pace in men than in women. Lung cancer mortality has declined by 54% since 1990 in men and by 30% since 2002 in women due to reductions in smoking, with the pace accelerating in recent years; from 2014 to 2018, the rate decreased by more than 5% per year in men and 4% per year in women (ACS, 2021a).
| Sex | Estimated New Cases | Estimated New Deaths |
|---|---|---|
| (ACS, 2021a) | ||
| Male | 119,100 | 69,410 |
| Female | 116,660 | 62,470 |
| Both sexes | 235,760 | 131,880 |
Disparities by Sex
Studies of more than 450,000 patients over a period of eight years have consistently shown that men experience lung cancers at a higher rate than women. Historically, this was due to the fact that men smoked much more than women. This has progressively become less so, to the point that the levels of smoking are equal between the two sexes. Regardless of the various confounding variables (lung cancer types, smoking histories, and socioeconomic backgrounds allowing access to care) men were consistently found to have a higher incidence of lung cancer than women (Tolwin et al., 2020).
Cultural and Ethnic Disparities
Recent statistics of rates of lung cancers among various races and ethnicities show the incidence between Black people and White people to be almost equal. The next most common occurrence is among American Indian/Alaskan Natives, followed by Asian/Pacific Islanders, and finally, Hispanics, at less than half the prevalence of Whites and Blacks (see table below).
| Race/Ethnicity | Rate per 100,000 |
|---|---|
| (ACS, 2021a) | |
| Non-Hispanic White | 62.6 |
| Non-Hispanic Black | 60.9 |
| American Indian/Alaskan Native | 52.7 |
| Asian/Pacific Islander | 34.4 |
| Hispanic/Latinx | 29.7 |
In a study of approximately 1,200,000 subjects, the measurement of metastatic presentation upon the diagnosis of non-small cell lung cancer (NSCLC) was remarkably similar across ethnic strata. The results showed that 47% of Black study subjects, 49.66% of Hispanic subjects, and 42.33% of White subjects originally presented to a physician or advanced practice provider with symptomatic complaints that were caused by stage IV disease with metastasis to another organ system (Aghdam et al., 2020).
Prevalence by Age
Lung cancer is predominantly a disease of the elderly. Incidence of new cases and overall prevalence jump dramatically in adults over the age of 50, with the highest rate of new cancers among those 80–84 years (CDC, 2021c). Generally, women develop lung cancer at a younger age than men. On the average, women with lung cancer live one year longer than men (Harding et al., 2020).
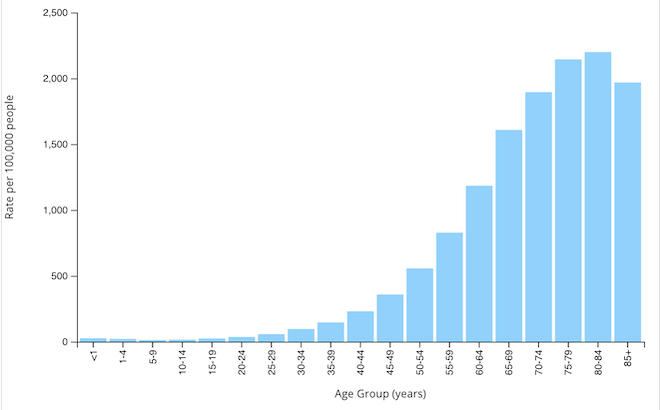
Rate of new lung and bronchus cancers by age group, U.S., 2019. (Source: CDC, 2021c).
LUNG CANCER AND LIFE EXPECTANCY
Due to the late stages of the cancer upon diagnosis, lung cancer has a high mortality and a low cure rate. These have improved somewhat in recent years because of less invasive surgical treatments such as video-assisted or robot-assisted thoracoscopy (VAT or RAT), more direct radiation therapy, and more effective systemic therapies (e.g., chemotherapy, immunotherapy, and targeted therapy) (Harding et al., 2020).